I’m on day 5 of an 8-day run of Port-and-Starboard trauma call (Navy talk for every other night) and am feeling my age. There was a time when I could do this for weeks at a time and still have the energy to play or go out with my wife. Now I drag home at the end of my off day and collapse into a snoring heap. It hasn’t helped that I’ve had an elective schedule with a couple of complex surgeries on the days when I wasn’t at the Trauma Center.
Aside from the physical toll this week has taken, there has been a mental struggle as well. I accept that I am a dinosaur and that the way that I approach the craft of surgery hearkens back to a bygone era when primary care doctors still saw their patients in the hospital, and surgeons accepted full responsibility for the postoperative care of the patients on whom they operated. I feel old when I find myself out of step with the current style of patient care.
I missed a critical meeting this morning at one hospital because I was up to my elbows in surgery at another. The meeting involved a discussion with a group of surgeons who believe that it is OK for their Physician’s Assistant to see their patients after surgery and only involve the surgeon when there is a problem. Even the usually laissez faire Medical Staff president had a hard time with that and wanted a regulation requiring surgeons to see patients for at least 48hrs postop. The fact that we need such a regulation is appalling to me. I had intended to speak out strongly, but patient care got in the way. I am awaiting word as to how the meeting turned out. But the mere fact that this is an issue leaves me feeling out of step and, well, old fashioned.
“Watching her bounce out of the operating room as we wheeled the patient to recovery, I remembered many of my own first times and smiled.”
Then there was the surgery that I was doing rather than attending the meeting. My patient had a gallstone stuck in her common bile duct, the tube connecting the liver to the intestine. An attempt to remove it endoscopically had failed yesterday, and so she needed surgical treatment. This is a procedure I have done hundreds of times. I’ve done it both with the laparoscope and with the old-fashioned open technique. On this particular morning I was working with a surgical resident at the Trauma Center. It came out in our discussion prior to surgery that the resident had never done any type of common duct exploration, either laparoscopic or open. I was mildly surprised. While the procedure is done much less frequently than when I was in training, I hadn’t thought it rare. By the time I was at this resident’s level I had done 20 to 30 common bile duct explorations and was by that time teaching the procedure to my juniors. But no, it seems the operation has become so uncommon that a fourth year surgical resident hasn’t even seen one. Again I felt my age. Times have indeed changed.
In the end, I was unable to get the stone out with the laparoscope and had to do a traditional open duct exploration. It went well, and the patient is recovering. The resident was tremendously excited, especially since I let her do much of the procedure herself. Watching her bounce out of the operating room as we wheeled the patient to recovery, I remembered many of my own first times and smiled. I may be an old curmudgeon, but I still enjoy teaching what I’ve learned.
Like What You’re Reading?!
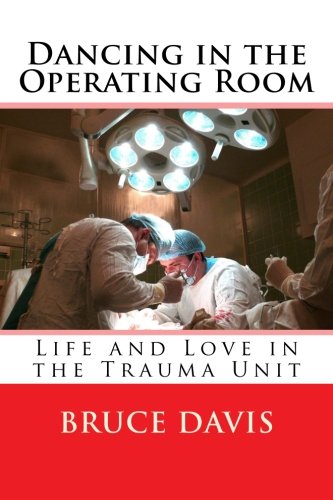
Get Dr. Davis’s new book, Dancing in the Operating Room, a collection of these and other short essays about life and love in the world of surgery and medicine, now available from Amazon in print or as an e-book. Check it out!


