According to recent estimates, about 400,000 pacemakers and implantable cardioverter defibrillators (ICDs) are surgically implanted each year in the United States. In 2008, the American College of Cardiology Foundation (ACCF), American Heart Association (AHA), and the Heart Rhythm Society (HRS) released guidelines for using device therapy to manage cardiac rhythm abnormalities.
Since the release of the 2008 guidelines, many clinical research advances relating to device-based therapies have emerged, says Andrew E. Epstein, MD, FAHA, FACC, FHRS. “In an effort to help clinicians keep pace with these advances, the ACCF, AHA, and HRS jointly released updated guidelines in 2012 for the use of device-based therapy in treating heart rhythm disorders. The guidelines can help in clinical decision making in most circumstances.”
The 2012 update writing group included experts in device therapy, cardiovascular care, internal medicine, cardiovascular surgery, and pediatric and adult electrophysiology. The guidelines were also developed in collaboration with the American Association for Thoracic Surgery, Heart Failure Society of America, and Society of Thoracic Surgeons.
Building on Earlier Cardiac Device Guidelines
For the 2012 update, the writing group began by reviewing the 2008 recommendations. The latter are largely unchanged for standard pacing and ICD indications. However, given new data on cardiac resynchronization therapy (CRT), the 2008 guidelines were updated with CRT as its focus, especially with regard to expanding indications for this treatment (Figure 1).
“CRT can significantly improve quality and quantity of life by delaying or avoiding worsening heart failure.”
“Despite our improvements in managing patients with device-based therapies, it can still be challenging for physicians to select patients in whom these devices will provide the most benefit,” explains Dr. Epstein, who was vice-chair of the writing committee for the guideline update. “Patients had previously been excluded from receiving CRT, but more recent studies have shown that select individuals who previously were not felt to be candidates for CRT can benefit from the intervention. For these patients, CRT can significantly improve quality and quantity of life by delaying or avoiding worsening heart failure.”
ECG Findings Matter
The guideline writing group has provided clear recommendations about which patients are most likely to benefit from CRT. Patients with mild heart failure or New York Heart Association class II should be considered for CRT based on results from ECGs. “When compared with patients whose ECG findings are normal, those with the most abnormal ECGs can potentially benefit most from CRT,” Dr. Epstein says. “In particular, patients with left bundle-branch block complexes at least 150 milliseconds in duration appear to benefit the most from CRT.”
The Right Device for the Right Patient
Dr. Epstein notes that it can be difficult for clinicians to assess the likelihood of success with CRT on a caseby- case basis. “Implanting pacemakers and ICDs is usually straight forward, but there is always the potential for complications. The key is to select the right device for the right patient and to monitor them closely after their procedure. This guideline update provides indications for the patients who are most likely to benefit from device therapies based on the best evidence to date.”
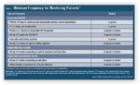
In addition, the 2012 guidelines provide other modifications to help physicians decide which patients with atrial fibrillation (AF) might benefit from CRT. In particular, CRT can benefit some patients with left ventricular dysfunction and AF. The committee also summarized the minimum frequency of in-person and remote monitoring of patients with cardiovascular implantable electronic devices (Figure 2).
Keeping Up to Date on Guidelines
The 2012 guideline update was published in the October 2012 issues of Circulation, the Journal of the American College of Cardiology, and the HeartRhythm Journal. Dr. Epstein recommends that clinicians refer to these guidelines when managing patients with cardiac rhythm abnormalities. “The updated guidelines extend and clarify current best practices, but will continue to evolve as technology advances,” he says. “More work is currently underway to develop a related ‘Appropriate Use’ document. The hope is that further interpretation of the best science available will enable us to apply the lessons learned in research studies to various clinical scenarios so that we can optimize outcomes in this growing patient population.”
Figure 2: Minimum Frequency for Monitoring Patients



 TimH
TimH