Published reports have shown that the number of total knee arthroplasty (TKA) procedures performed in the United States more than tripled from 1993 to 2009, while the number of total hip arthroplasty (THA) surgeries doubled during the same timeframe (Figure 1). “In the setting of healthcare reform and cost containment initiatives, increasing surgical volumes have gained greater attention,” says Peter B. Derman, MD, MBA. Several explanations have been proposed regarding the increasing prevalence of total joint arthroplasties, and it is likely that a multitude of interacting factors play a role. These include obesity, the aging population, supplier-induced demand, and changing expectations about the quality of an active lifestyle, among other factors.
Observational studies have described various trends in arthroplasty, examining its economic ramifications as well as projecting future utilization. Dr. Derman and colleagues conducted a study, published in the Journal of Bone & Joint Surgery, to further the understanding of why there has been a more rapid growth in TKA when compared with THA. “The increasing incidence of overweight and obesity was of particular interest to us,” says Dr. Derman. “Studies have linked high BMIs with an elevated risk of knee arthritis, but this relationship is less robust with respect to the hip. We postulated that this differential effect might explain why knee replacement volumes are growing faster than hip replacement volumes.”
Weight & Age
For the analysis, Dr. Derman and colleagues used data obtained from the Nationwide Inpatient Sample on TKA and THA volume, length of hospital stay, and in-hospital mortality. The sample included details on over 8 million admissions at more than 1,000 hospitals in 44 states. The authors analyzed clinical, demographic, and economic factors from 1993 to 2009 that have been linked to the growth in joint replacement procedures.
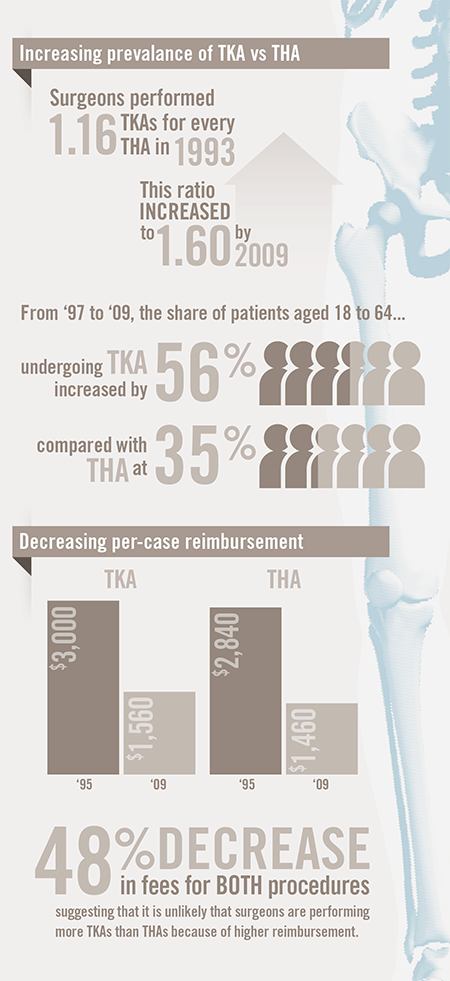
In 1993, surgeons performed 1.16 TKAs for every THA, but this ratio increased to 1.60 by 2009. There was more rapid growth in the utilization of TKA over THA in individuals with BMIs of 25 kg/m2 or higher, while TKA and THA grew proportionately in patients with non-elevated BMIs. Of the factors examined in the study, BMI played the most substantial role in increasing demand for TKA above that of THA. “An increase in the prevalence of overweight and obesity in the U.S. accounted for 95% of the differential increase in TKA over THA volumes,” Dr. Derman says (Figure 2).
The study also found that patients aged 18 to 64 experienced a more rapid rise in rates of overweight and obesity when compared with those older than 65. From 1997 to 2009, the share of patients aged 18 to 64 undergoing TKA increased by about 56%, compared with a rate of 35% for THA.
Financial Considerations
Results also showed that hospital and physician reimbursement, length of stay, and in-hospital mortality did not appear to improve more for TKA than THA during the study period. Surgeon per-case reimbursement for TKA decreased from about $3,000 in 1995 to $1,560 in 2009, and surgeon fees for THA dropped from $2,840 to $1,460. This represents an approximately 48% decrease in fees for both procedures, suggesting that it is unlikely that surgeons are performing more TKAs than THAs because of higher reimbursement.
The surgical community appeared to respond to the additional demand primarily by increasing per-physician output rather than by increasing labor supply. “Our observed differential growth rate in TKA procedures could not be attributed to changes in physician or hospital payments, length of stay, in-hospital death rates, or surgical workforce characteristics,” says Dr. Derman.
Important Implications
Dr. Derman notes that if overweight and obesity rates continue to climb, clinicians should expect a greater acceleration in the number of TKAs performed annually in the U.S. and a more modest increase in THA volumes. “This knowledge is important because it can inform future policy decisions regarding healthcare funding and surgical workforce training and may help guide the allocation of preventative health resources,” he says. Furthermore, this knowledge may increase clinicians’ understanding and planning for future arthroplasty trends.
Weight loss is already routinely recommended by physicians for relief and prevention of arthritic pain. Dr. Derman says it can also make joint replacement surgeries less technically demanding and lead to better recovery. “Investing in obesity interventions can be beneficial for a wide range of health issues,” he says. “It’s possible that future research will suggest that greater efforts to encourage weight loss can decrease the utilization of TKA and THA.”


 TimH
TimH