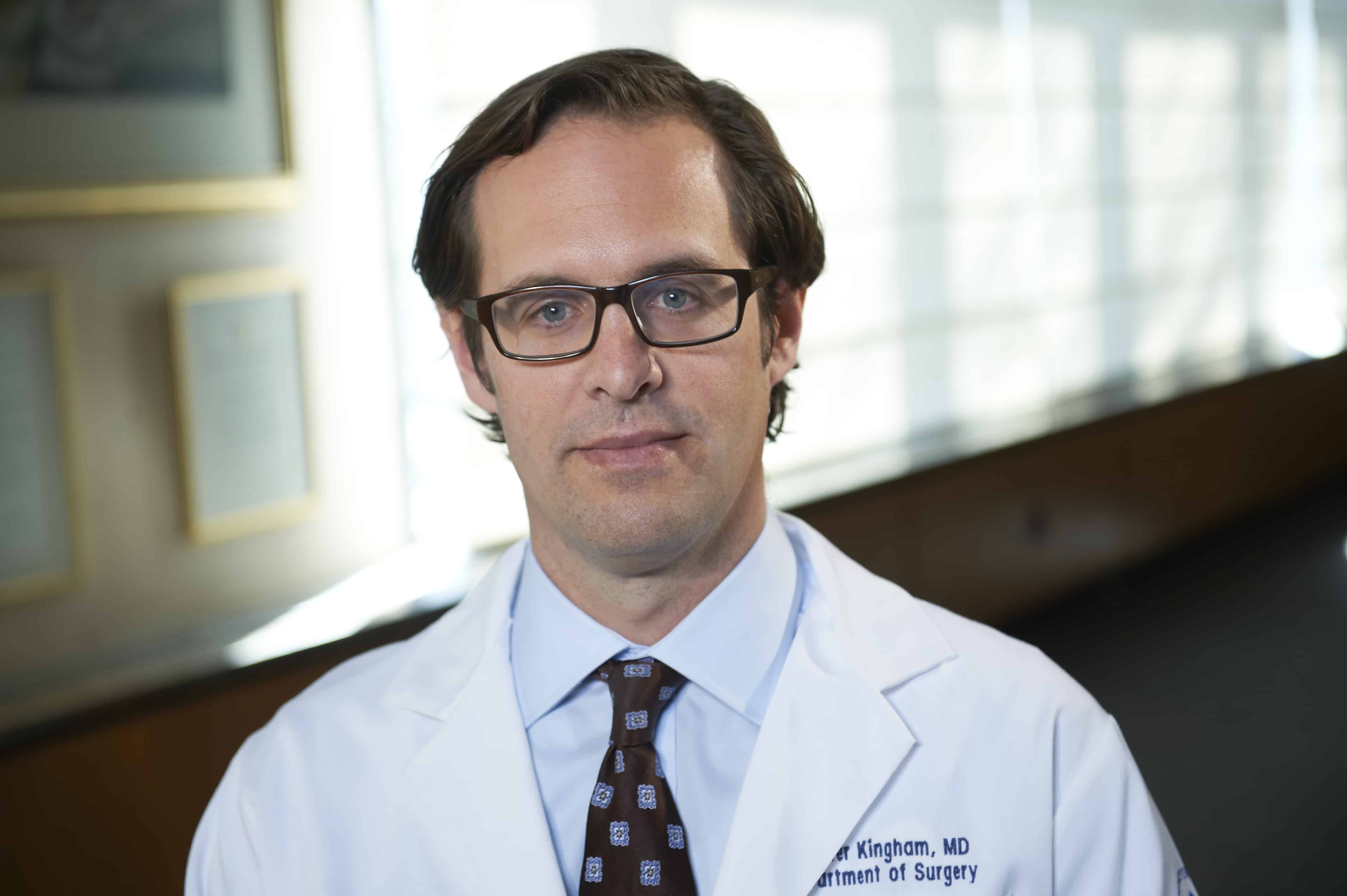
Research has shown that the 5-year survival rate among patients with cancers of the liver undergoing resection is high. Many candidates, however, will not undergo these procedures because of the high morbidity and mortality risk associated with them. “Over the past 20 years, liver cancer surgery has become safer and more effective,” explains T. Peter Kingham, MD, FACS. “One of the reasons for this has been advances in surgical treatment.” Specifically, there has been greater use of hepatic parenchymal preservation, a surgical approach in which less liver is resected. These procedures can benefit patients with single tumors or multiple tumors confined to one side of the liver.
Analyzing Changes in Outcomes
In a study published in the Journal of the American College of Surgeons, Dr. Kingham and colleagues at Memorial Sloan Kettering (MSK) Cancer Center analyzed the correlation between hepatic resection, mortality, and complication rates using data compiled over 19 years. They analyzed hospital records of all patients who underwent both major and minor hepatectomy for a malignant liver cancer diagnosis at MSK. Patients were divided into three equal groups according to time period: early (1993-1999), middle (2000-2006), and late (2007-2012). Surgical morbidity and mortality rates were then compared between the time periods.
According to the results, the 90-day mortality rate decreased over the three time periods from 5% to less than 2% for all patients involved in the analysis. Overall, the complication rate dropped from 53% to 20%. “The number of major hepatectomies decreased from two-thirds of cases to about one-third,” Dr. Kingham adds. The transfusion rate and liver dysfunction also decreased significantly over the study period. Interestingly, the mortality risk for major hepatectomies remained the same in all three time periods. This suggests that the improved outcomes were related specifically to greater use of parenchymal preservation procedures.
“Our findings suggest that outcomes are improving because we’ve been able to preserve more of the liver without compromising the oncologic principles of liver surgery,” Dr. Kingham says. “By preserving the liver, we put less physical stress on the patient’s body, giving them a chance to recover more quickly. It also gives surgeons the option to perform another surgery if the cancer recurs.”
Assessing the Implications
Many liver cancer patients are never referred to surgeons because of the impression that hepatectomy is too dangerous and outcomes are poor. Dr. Kingham says that the emergence of parenchymal preservation and other advances should change these perceptions. “Procedures like parenchymal preservation are helping reduce morbidity and mortality,” he says. “Our findings may help when making treatment decisions with liver cancer patients. Surgeons should also consider refocusing their plans for resections to remove less liver without being concerned about compromising outcomes.”


 admin
admin