Major lower-extremity amputation remains a commonly performed procedure in the United States, and studies estimate that the number of Americans who will be living with a major amputation will exceed 3.6 million by 2050, with the majority of these cases being attributable to vascular conditions. Amputation for lower-extremity arterial disease has been associated with substantial postoperative mortality and morbidity due to the inherent medical comorbidities. Risk factors associated with mortality after major amputation include older age, cardiac and pulmonary disease, renal insufficiency, steroid use, dependent functional status, and preoperative sepsis.
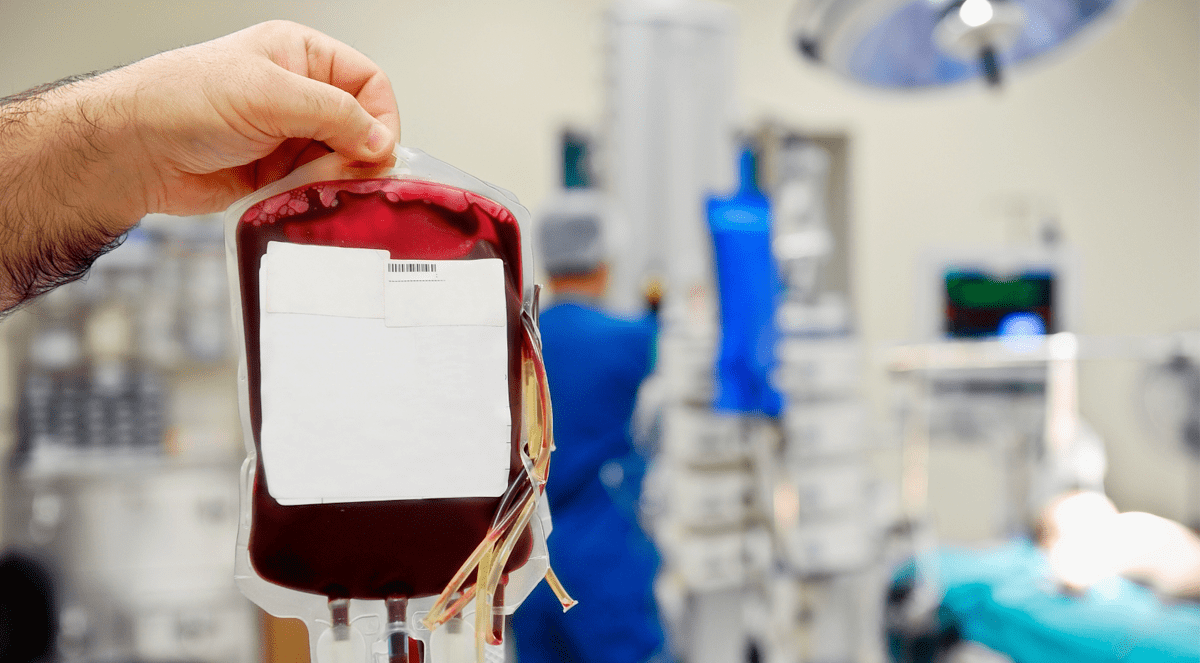
“Research indicates that perioperative packed red blood cell (RBC) transfusions are often administered to patients with vascular disease, but the effect of this treatment on postoperative survival and outcomes among patients undergoing amputation is poorly understood,” says Tze-Woei Tan, MD, MBBS, FACS, RPVI. Despite its potential advantages in critically ill patients with acute cardiac events, RBC transfusions have been linked to higher mortality in patients undergoing various surgeries as well as perioperative wound infection and pneumonia. In patients undergoing lower-extremity bypass, RBC transfusion can increase risks for surgical site infections and early bypass graft thrombosis.
New Data
For a study published in Surgery, Dr. Tan and colleagues evaluated the outcomes of patients undergoing major lower-extremity amputations who received perioperative packed RBC transfusions. The authors used the dataset of the National Surgical Quality Improvement Program (2005–2011) to examine more than 5,700 above-knee and over 6,700 below-knee amputations. Study participants were then stratified by perioperative RBC transfusion and assessed for outcomes, including perioperative mortality, myocardial infarction, thromboembolism, and duration of stay at the hospital.
“Results showed that about 17% of the more than 12,000 amputations observed in our study cohort required packed RBC transfusions,” Dr. Tan says. The majority of RBC transfusions were given either within 72 hours preoperatively or intraoperatively. Some received transfusion postoperatively. Most cases—66%—were performed for critical limb ischemia. The overall 30-day mortality was about 9% and significantly higher for those undergoing above-knee amputations.
“Among patients who had major lower-extremity amputation, perioperative RBC transfusion independently predicted greater risks for perioperative pneumonia, thromboembolism, and prolonged hospital stays,” adds Dr. Tan. “It’s important to note that patients who undergo amputation and require RBC transfusions are generally sicker, meaning that they will require close monitoring before, during, and after their operation.”
In an analysis of a crude and risk-adjusted group frequency–matched cohort, RBC transfusion during amputation was linked to a significantly higher risk of nosocomial pneumonia, surgical site infection, and thromboembolism. The hospital stay also was longer for patients undergoing RBC transfusions.
Considering Implications
The findings have important implications because the practice of perioperative RBC transfusion has been under increased scrutiny. Most published guidelines recommend a restrictive RBC transfusion strategy even in the most acutely ill patients. “Ongoing vigilance is needed when managing patients undergoing amputations during the perioperative period to ensure that outcomes are optimized,” says Dr. Tan. The study notes that the findings further support the notion that RBC transfusions have deleterious effects and emphasize the importance of using restrictive transfusion practices in patients undergoing amputation.


 PWeekly
PWeekly