Frail surgery patients are at greater risk of death and poor outcomes after their procedure than other patients. Recognition of frailty and its associated risks is important because it can inform shared decision making and may help identify candidates for palliative care consultation. Some institutions have started implementing quality improvement (QI) initiatives to screen patients who are scheduled for elective surgery for frailty. The purpose of such initiatives is to identify patients at high risk for postoperative mortality and morbidity.
Examining a QI Initiative
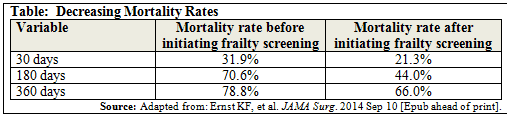
In 2011, Jason Michael Johanning, MD, MS, and colleagues at the Omaha VA Medical Center implemented a QI initiative to actively encourage preoperative palliative care consultation in frail patients. They then conducted a study—published in JAMA Surgery—that examined the effects of a system-wide frailty-screening program on palliative care consultation and patient mortality. The investigators evaluated 310 palliative care consultations that were ordered for surgical patients, 160 of which were from before the QI program was implemented and 150 were from after program initiation. Dramatic decreases in mortality rates were seen at 30, 180, and 360 days after initiating the frailty-screening program (Table).
Consults Before Surgery
It is important to engage older, frail patients in palliative care discussions before surgery, according to Dr. Johanning. “Obtaining a palliative care consult before surgery didn’t appear to increase mortality risks,” he says. “Instead, they had a protective effect. Overall, our data demonstrate that a frailty-screening program can alter the pattern and timing of palliative care consultations.”
Dr. Johanning notes that the proportion of consultations ordered by surgeons increased after the QI program was introduced and consultations were more likely to be made before surgery, with equal numbers of consultations occurring during the preoperative and postoperative period. “The strongest predictor associated with reduced mortality was when surgeons ordered a preoperative palliative care consultation,” he says. The data showed that one death was prevented for every three surgeon-ordered preoperative consultations.
Raising Awareness
According to Dr. Johanning, the study findings should reassure physicians who fear that preoperative palliative care consultations may increase mortality by steering patients away from beneficial surgical treatment. “Our study raises awareness on the importance of identifying high-risk patients with frailty screenings,” Dr. Johanning says. “There are ways to partner with palliative care rather than work as adversaries in the postoperative period. The key is to address objective surgical risk by clinicians on both medical and surgical services prior to an operation to encourage shared decision making.”


 Janine Anthes
Janine Anthes