Symptoms of infection with the Zika virus in Brazil may be masked by simultaneous infection with other mosquito-spread viruses common in the same region—such as dengue fever and chikungunya viruses—pointing to the need for comprehensive testing, according to a study led by a UCSF expert in DNA-based diagnostics in collaboration with Brazilian researchers.
Using sophisticated genetic fingerprinting techniques that can identify multiple co-infections, a research team led by Charles Chiu, MD, PhD, associate professor of laboratory medicine and of medicine, and director of the UCSF-Abbott Viral Diagnostics and Discovery Center at UCSF, found two cases of co-infection with the chikungunya virus among 15 previously confirmed Zika cases from the state of Bahia, Brazil, diagnosed from April 2015 to January 2016.
“With these viruses, the symptoms associated with acute illness, including fever, rash, joint pains and conjunctivitis, are non-specific, so it is difficult to make an accurate diagnosis based on clinical findings alone,” Chiu said. “It’s easy to imagine a physician failing to detect Zika when they instead suspect a different virus that causes similar symptoms, and then their suspicion is confirmed by a diagnostic test designed to detect only that virus – they might easily miss a co-infection if they do not test for more than one virus.”
Curtailing an Outbreak
In most cases of infection, Zika itself causes no symptoms or relatively minor symptoms.
In a collaboration with Silvia Sardi, PhD, of the Federal University of Bahia, one of the first scientists to identify Zika as the cause of the Brazilian outbreak, Chiu used a single “metagenomic” laboratory test that can detect virtually any known virus to analyze blood samples from patients infected with Zika. The study was published online ahead of print on July 13 in the Journal of Clinical Microbiology.
In a related study using serum from the same cases, published concurrently in Emerging Infectious Diseases, Chiu and colleagues determined by “molecular clock” sequencing analysis that the Zika strain circulating in Bahia likely emerged in mid-2014, more than eight months before the first documented case of Zika infection in Brazil was reported in March of 2015.
Bahia is the state with the greatest number of Zika-associated cases of microcephaly, in which the brain and head of a child does not develop normally as a result of infection of the mother early in pregnancy.
“The failure to identify Zika virus in Brazil in a timely fashion underscores the urgent need for comprehensive diagnostic tests that can rapidly monitor the emergence of outbreak pathogens,” Chiu said. “Had these tests been in place, we might have had the opportunity to curtail spread of the outbreak.”
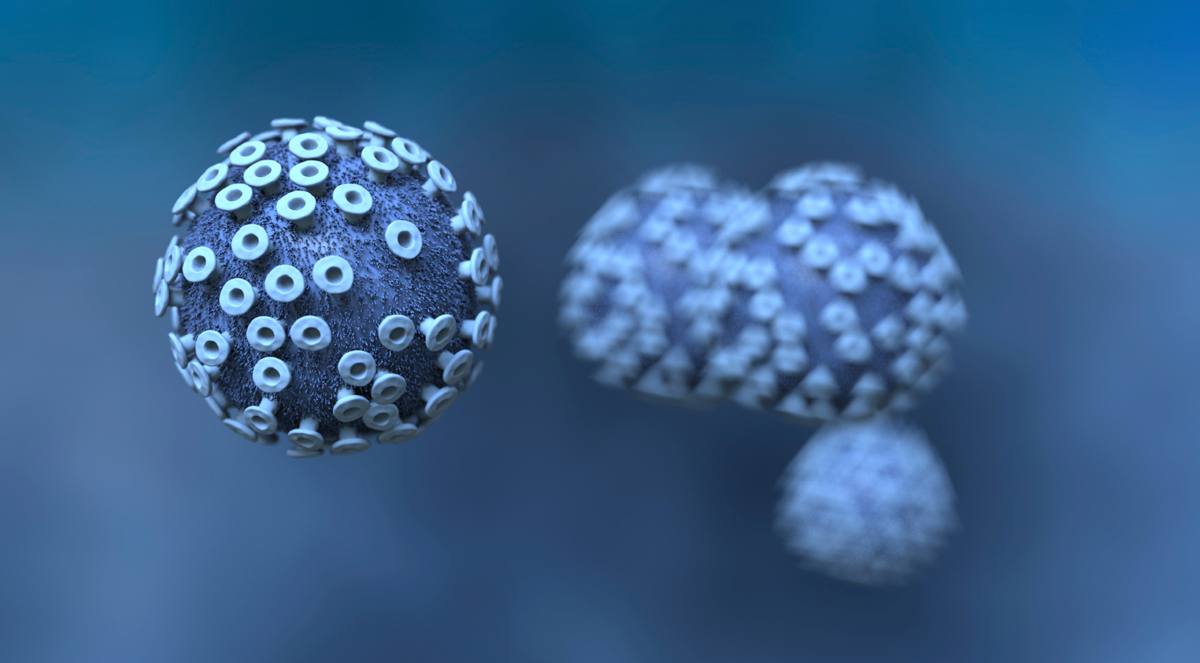
Both Zika and chikungunya viruses have only recently spread to the Western Hemisphere, but dengue, which was not observed in the study cohort of 15 patients, has been endemic in Latin American countries for many years. In the Americas, the mosquito Aedes aegypti is the most common vector of Zika, dengue and chikungunya. The researchers did not detect telltale genetic fingerprints pointing to co-infection with other common tropical mosquito-borne pathogens, such as the malaria parasite, in any of the samples.
Growing Problem in the U.S.
Aedes aegypti is frequently found as far north as Florida and the Gulf Coast. Mosquito-borne dengue and chikungunya cases have originated in Florida in recent years. Scientists predict that that there will be mosquito-borne Zika cases originating within the United States. In addition, infected men can transmit Zika virus through sex. Zika survives in semen longer than in blood, but it is unclear for how long.
Based on data from Brazil, a study published by researchers from the U.S. Centers for Disease Control and Prevention (CDC) in the July 7 edition of the New England Journal of Medicine roughly estimated the risk of microcephaly among children born to women infected with Zika during the first trimester to be as high as 13 percent. Zika infection has also been associated with immune responses that trigger Guillain-Barré syndrome, in which nerve damage causes limb muscle weakness, usually temporarily.
Prompt diagnosis of chikungunya and dengue also remains important, Chiu said, as these infections can also lead to longer-lasting medical problems in some cases. Chikungunya infection can cause chronic arthritis, while infection with the dengue virus can cause encephalitis, immune-mediated syndromes and stroke.
Currently No FDA-Approved Test for Zika
There is no test for Zika virus that has been licensed by the U.S. Food and Drug Administration. The lab tests most often used today detect antibodies to Zika, but often are non-specific and can give a positive reading following infection with dengue or chikungunya, making the result unclear. Another type of test detects Zika viral genes within about a week of infection.
The results of these studies suggest that co-infection during the ongoing Zika virus outbreak with a wide range of different viruses is not common, and that a test able to detect Zika, chikungunya and dengue simultaneously would be sufficient for the current outbreak, Chiu said. But Chiu believes that continued technological advances in next-generation sequencing will eventually make broad-based metagenomic testing for any pathogen feasible, perhaps even in the field.
“Traditionally, barriers to next-generation sequencing have included high costs, complex instrumentation, and lack of dedicated bioinformatics tools,” the researchers state in the journal article. “These barriers are being overcome with the development of rapid computational pipelines for analysis of next-generation sequencing data, and emergence of portable sequencers that can be used in field laboratories and other point of-care settings.”
Source: UCSF.