Alborz Sherafati, MD, MS
Limited research has been done on outcomes after the return of secondary findings in large-scale sequencing projects. To assess this in the setting of hypercholesterolemia, Alborz Sherafati, MD, MS, and colleagues examined 1-year outcomes after the return of results (RoR) on pathogenic/likely pathogenic (P/LP) variants associated with familial hypercholesterolemia (FH) in phase 3 of the eMERGE network from 2015-2019.
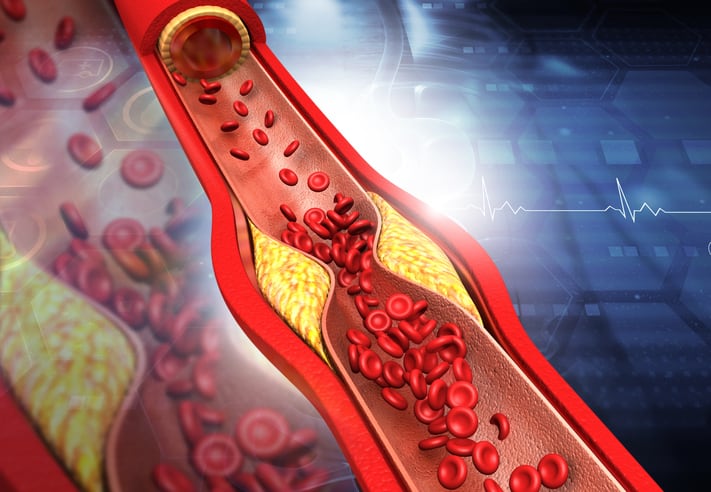
The prospective cohort study included adult participants (N=18,544) at seven sites. Dr. Sherafati and colleagues examined “the clinical impact of returning results from targeted sequencing of 68 actionable genes, including LDLR, APOB, and PCSK9.” They obtained information on process, intermediate, and/or clinical outcomes within 1 year of the RoR through EHR review.
“A process outcome was defined as referral to a specialist or ordering new tests, including lipid profile and screening tests for coronary heart disease,” the researchers wrote. “An intermediate outcome was defined as [a] new diagnosis of FH or atherosclerotic cardiovascular disease. A clinical outcome was defined as initiation or change in lipid-lowering medication. The primary outcomes were a new diagnosis of FH and modification of lipid lowering therapy.”
RoR Increases Outcomes for Nearly All Participants
In total, 134 participants received a return of results, and data for the outcome analysis were available for 119 individuals.
Process (86%), intermediate (49%), and/or clinical (26%) outcomes were documented in 92% of participants. Process outcomes included orders for new tests (72%) and referral to a specialist (61%). Prior to RoR, 86.5% of participants with FH-associated P/LP variants had received a diagnosis of hypercholesterolemia, but only 17.6% had a diagnosis of FH; in addition, 89% were on a statin but only 58% were being treated with a high-intensity statin.
Following RoR, 44% received a new diagnosis of FH. Lipid-lowering therapy was adjusted in 26%, including the initiation of a statin in 5%, increasing a statin dose in 13%, and adding ezetimibe or a proprotein convertase subtilisin/kexin type 9 inhibitor in 12.6%.
“These results highlight the clinical utility of returning FH variants in EHR-linked biobanks,” Dr. Sherafati and colleagues wrote.