The American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology (ACE) Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis – 2016 Update and Algorithm were published in September 2016.
Most recently, the American College of Physicians (ACP) published new osteoporosis guidelines (View or Download PDF, and although AACE/ACE commends the ACP effort in addressing the importance of identifying and managing osteoporosis and fracture risk in postmenopausal women and older men, important differences from the AACE/ACE guidelines need to be clarified.
View or Download 2020 Algorithm (PDF)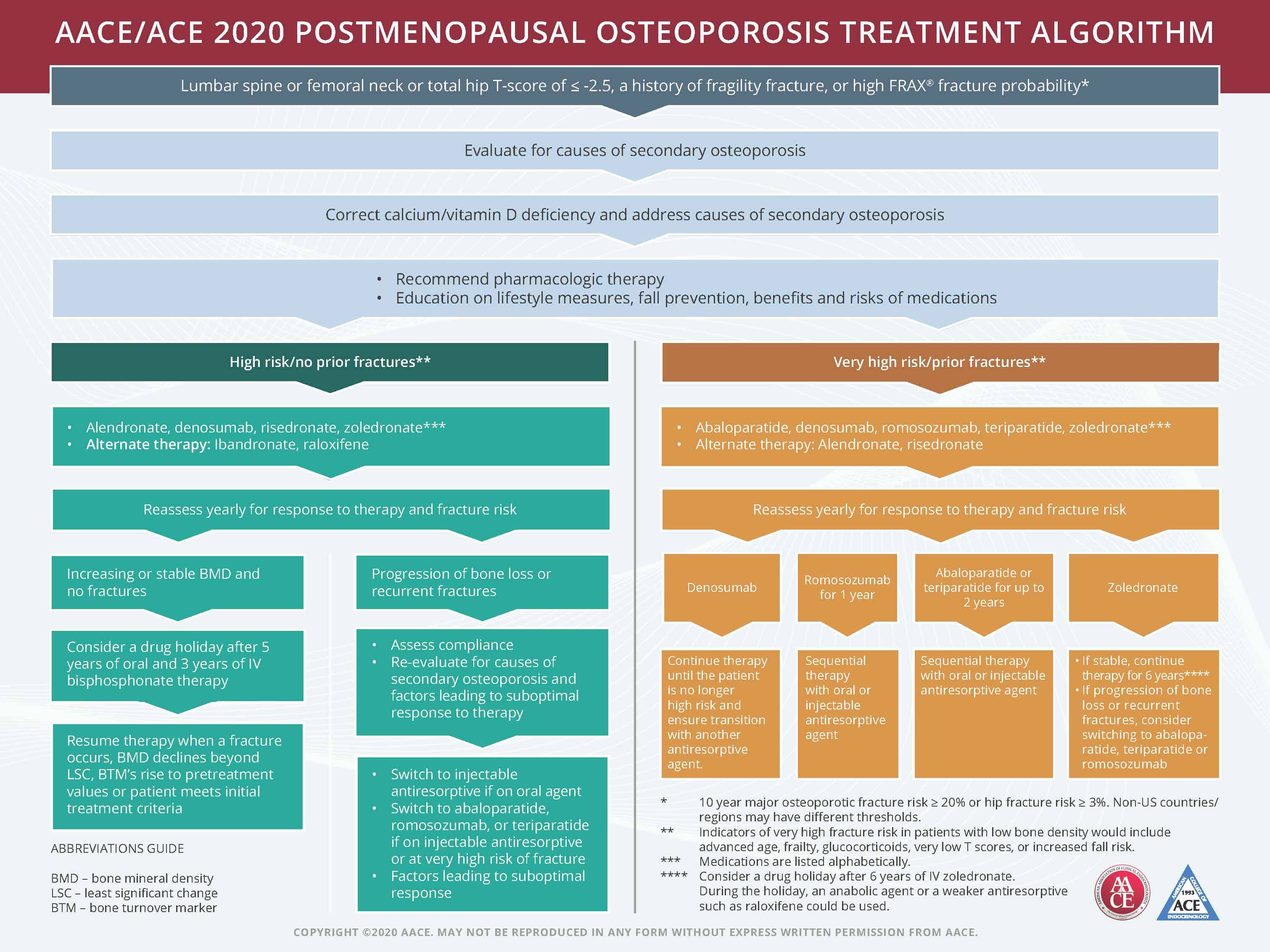
The recommendations in all AACE/ACE Guidelines reflect not only the latest evidence-based science, but also clinical experience and expert opinion, based upon the 2010 and 2014 AACE protocols for standardized production of clinical practice guidelines.
Antiresorptive pharmacotherapy has demonstrated efficacy for fracture risk reduction, but there is also a significant role for anabolic therapy in the treatment of osteoporosis, particularly in patients with severe osteoporosis and those who have clinical fractures during antiresorptive use.
The duration of therapy needs to be individualized. The recommendation for 5 years of therapy may be appropriate for some, but not for other patients. It is also important to note that drug holidays are not recommended for those on denosumab since the protection from vertebral fracture may be lost within 3-18 months after discontinuation.
AACE/ACE guidelines recommend that after the initiating therapy, patients should be reassessed with dual energy absorptiometry (DXA) bone mineral density (BMD) every 1 to 2 years until findings are stable, with continued interval monitoring depending on clinical circumstances. Thus, the frequency of BMD re-evaluation needs to be individualized. Obtaining a follow up DXA scan to identify individuals who are not responding to therapy is crucial to be able to change therapy before the occurrence of a clinical fracture that could be life altering.
These individuals often have undiagnosed disorders contributing to bone loss, or may have absorption or adherence issues. To this point, the ACP Recommendation 4, “ACP recommends against bone density monitoring during the 5-year pharmacologic treatment period for osteoporosis in women,” is noted as not having a strong evidence base (“Grade: weak recommendation; low-quality evidence”).
Raloxifene is not recommended for use in the ACP guidelines. Although raloxifene is not effective in reducing hip fracture risk, the AACE/ACE guidelines indicate that it may be appropriate initial therapy in some women who require only spine-specific therapy. For women at high risk of spine fracture but not at risk for hip or nonvertebral fractures, raloxifene may be appropriate, especially when other antiresorptive drugs are not tolerated or contraindicated, and for patients seeking a potential additional “benefit” of reducing breast cancer risk.
AACE/ACE agrees with the American Society for Bone and Mineral Research (ASBMR) statement that the ACP osteoporosis guidelines “fall short” in key tenets of osteoporosis treatment and management, specifically in the area of frequency of bone mineral density monitoring, treatment with anabolic agents, and the duration of therapy for the antiresorptive agents.
AACE/ACE guidelines provide the physician and advanced care providers with clinically relevant knowledge to help prevent fractures in postmenopausal women with increased fracture risk.
Source: AACE
Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocr Pract. 2020;26(1):1-46.