DENVER—The newest treatment for individuals diagnosed with Alzheimer’s disease (AD)—aducanumab (Aduhelm)—requires clinicians skilled in detection and recognition of early cognitive decline, as well as clinical resources that meet the needs of specialized care, according to recommendations issued by an expert panel.
The panel presented the recommendations at the Alzheimer’s Association International Conference.
The recommendations were also published online in the Journal of Prevention of Alzheimer’s Disease. In that article, Jeffrey Cummings, MD, Joy Chambers-Grundy Professor of Brain Science and director of the Chambers-Grundy Center for Transformative Neuroscience at University of Nevada, Las Vegas, summarized the key recommendations of the panel:
- Appropriate Patient Selection: The pivotal trials included patients with early Alzheimer’s who had confirmed brain amyloid using amyloid positron tomography or cerebrospinal fluid findings consistent with Alzheimer’s disease. The Expert Panel recommends that use of aducanumab be restricted to this population, in which efficacy and safety have been studied.
- Treatment Management: Aducanumab is titrated to a dose of 10 mg/kg over a 6-month period. The Expert Panel recommends that aducanumab be titrated to the highest dose to maximize the opportunity for efficacy.
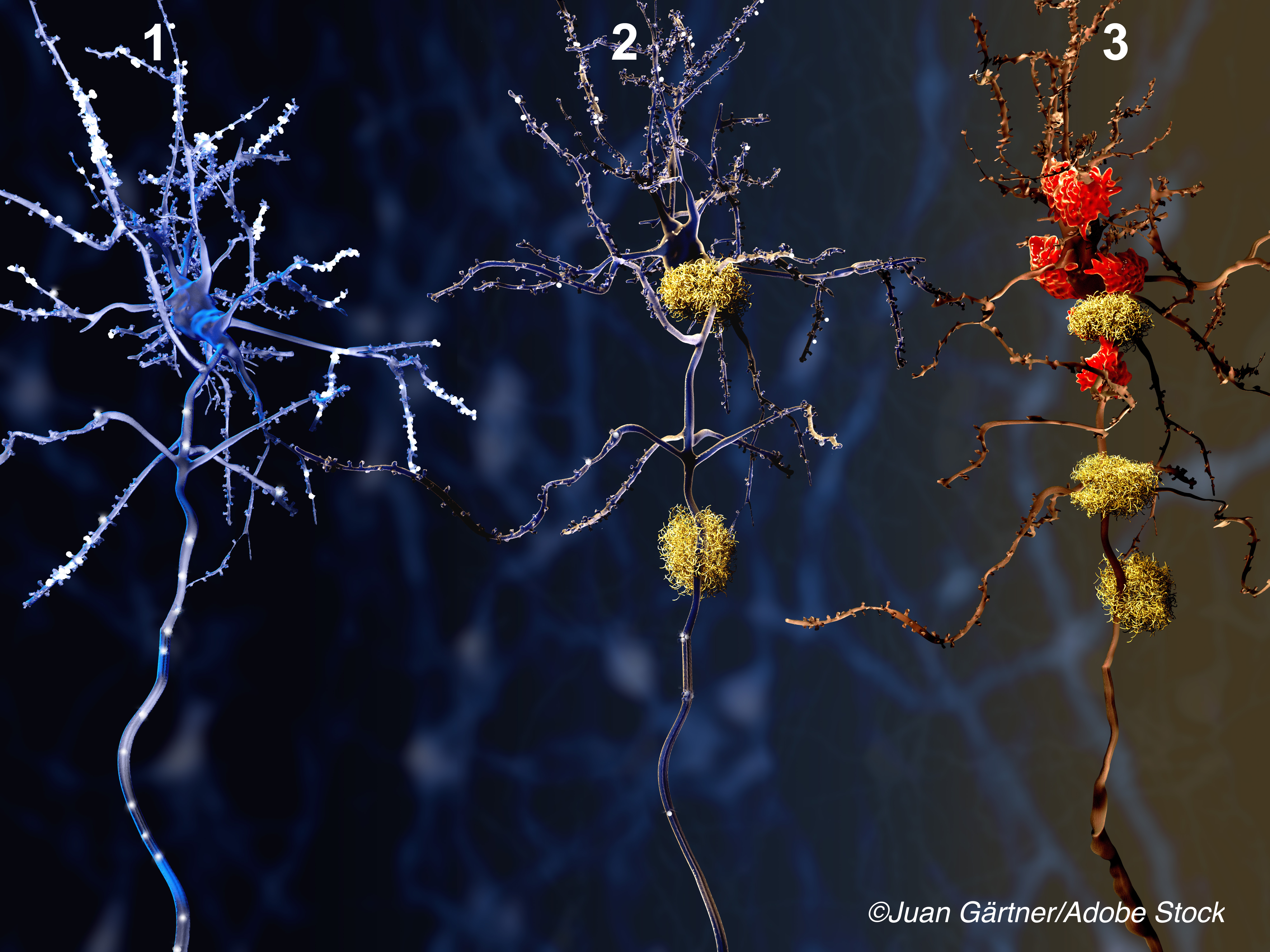
- Safety Monitoring: Aducanumab can substantially increase the incidence of amyloid-related imaging abnormalities (ARIA) with brain effusion or hemorrhage. The Expert Panel recommends MRIs prior to initiating therapy, during the titration of the drug, and at any time the patient has symptoms suggestive of ARIA.
- Patient Engagement: The Expert Panel emphasized the critical importance of engaging in a process of patient-centered, informed decision-making that includes comprehensive discussions and clear communication with the patient and care partner regarding the requirements for therapy, the expected outcome of therapy, potential risks and side effects, and the required safety monitoring, as well as uncertainties regarding individual responses and benefits.
“Aducanumab is a new treatment for Alzheimer’s disease,” Cummings wrote in the journal. “It provides opportunities and challenges for its introduction into management of AD patients. Aducanumab requires substantial infrastructure for appropriate administration: expert clinicians skilled in recognition of early Alzheimer’s; amyloid PET or lumbar puncture capability; experts in amyloid PET interpretation or cerebrospinal fluid analysis; infusion center availability; and access to MRI and experts in recognition and management of ARIA. Genetic counseling may be required in some circumstances, and all patients and care partners require education and support.
“Building this infrastructure for the appropriate use of aducanumab will require time, resources, and creative planning,” he suggested. “Appropriate use of aducanumab requires a commitment to patient-centered care and best practices for the safe delivery of this new treatment.”
In commenting on the recommendations by the expert panel, Maria C. Carrillo, PhD, Alzheimer’s Association chief science officer, told BreakingMED, “It is a new era in Alzheimer’s treatment and care. With the accelerated approval of aducanumab, people living with Alzheimer’s have a new treatment option.
“Not unexpectedly, clinicians nationwide are requesting clarity and more specific information about the appropriate use of this new treatment,” she said, noting that one session at the international conference was dedicated to how to use the new medication, designed to lower the amyloid burden on patients—considered a key element in the development and progression of Alzheimer’s.
“Now, an expert panel has published the first recommendations for the appropriate use of aducanumab,” Carrillo said. “The recommendations are needed because Alzheimer’s is a complex disease to identify, diagnose, and treat, and aducanumab is a first-in-class therapy. The recommendations are meant to fill the gap between the FDA Prescribing Information and the real-world implementation of this treatment.
“According to the authors, the recommendations are meant to assist practitioners in using aducanumab safely. That said, they do not replace clinician judgement in the delivery of care to individual patients,” she added.
Carrillo noted that, “the panel recommendations, the sessions at the conference, and the constructive response to them from the field, will be the basis for additional tools to educate and support clinicians, both primary care physicians and dementia specialists.”
“Clinicians are requesting clarity and more specific information about the appropriate use of this new treatment,” said Cummings. “The goal of the ’Aducanumab: Appropriate Use Recommendations’ is to provide guidance for the safe and effective use of this new drug, in particular because aducanumab is an unprecedented therapy. It is the first drug approved for treatment of Alzheimer’s based on amyloid plaque removal, addressing the underlying biology of the disease.”
“Many details of the clinical use of this new agent are not in the FDA’s Prescribing Information,” he added. “The recommendations fill the gap between the Prescribing Information and the real-world implementation of this treatment. How to choose appropriate patients, safely scale up to the full dose, monitor side effects, and assess effectiveness are all described. Plus, we address when to stop therapy and what patients should not receive this drug.”
The other panel members were:
- Paul Aisen, MD, Alzheimer’s Treatment Research Institute, University of Southern California, San Diego.
- Liana Apostolova, MD, Departments of Neurology, Radiology, Medical and Molecular Genetics, Indiana University School of Medicine, Indianapolis.
- Alireza Atri, MD, PhD, Banner Sun Health Research Institute, Banner Health, Sun City, Arizona.
- Stephen Salloway, MD, Butler Hospital and Warren Alpert Medical School of Brown University, Providence, Rhode Island.
- Michael Weiner, MD, Departments of Radiology and Biomedical Imaging, Medicine, Psychiatry and Neurology, University of California San Francisco.
Yet, regardless of the recommendations, controversy continues to track aducanumab. For example, in a move timed to coincide with the AAIC meeting, The New England Journal of Medicine published two perspectives and a letter on the subject of aducanumab.
In his perspective, titled “Controversy and Progress in Alzheimer’s Disease—FDA Approval of Aducanumab,” Gil D. Rabinovici of the Weill Institute for Neurosciences, University of California San Francisco, San Francisco, pointed out that the drug is not only the first Alzheimer’s treatment approved in 20 years, but also, “as a monoclonal antibody targeting aggregated beta-amyloid, it is the first approved drug to directly modify a core molecular feature of the diseases’s pathophysiology.” Nonetheless, Rabinovici pointed out that the evidence supporting its efficacy is less than overwhelming, since evidence from trials was conflicting and 40% of patients receiving high dose aducanumab developed vasogenic edema and cortical microhemorrhages versus 10% of controls, a toxicity that was safely managed in the trials. Finally, the drug is expensive—the estimated cost is $56,000 per year.
G. Caleb Alexander, MD, of the Center for Drug Safety and Efficacy at Johns Hopkins Bloomberg School of Public Health in Baltimore was one of seven authors—six of whom served on the FDA Peripheral and Central Nervous System Drugs Advisory Committee Meeting, which voted Nov. 6, 2020, to recommend that the FDA not move ahead with marketing approval of aducanumab—of a perspective that called the FDA’s July 7 accelerated approval a “regulatory failure.” Alexander et al applauded a decision by the FDA’s interim commissioner to call for an Office of Inspector General investigation of the approval. They noted, “…we believe such an investigation should be expeditiously performed, so as to learn how this regulatory failure occurred and to ensure that it doesn’t occur again. Though the decision will reverberate for years, early signs of its gravity are already reflected in announcements by two other manufacturers that they will seek accelerated approval for Alzheimer’s treatments on the basis of amyloid as a surrogate.”
But four FDA researchers—Billy Dunn, MD, Peter Stein, MD, Robert Temple MD, and Patrizia Cavazzoni, MD—in a letter to NEJM, defended the FDA’s action as appropriate and clinically warranted. They noted that FDA has not previously endorsed amyloid reduction as an appropriate biomarker for efficacy, but they cited “…the full range of data, particularly recent data, from monoclonal antibody programs targeting amyloid, which supports using amyloid reduction as a ’reasonably likely’ surrogate.”
The FDA researchers concluded that aducanumab “was approved under statutory and regulatory provisions that allow ’Accelerated Approval’ of drugs intended for serious or life-threatening conditions lacking adequate available therapies on the basis of an effect on a surrogate end point that is ’reasonably likely’ to predict clinical benefit—reasonably likely, not certain. Aducanumab met these elements: Alzheimer’s is a serious disease with substantial unmet need; aducanumab targets the underlying pathophysiology, unlike available therapies; there is compelling evidence that it reduces plaque; and this reduction by a monoclonal antibody targeting aggregated amyloid is reasonably likely to predict clinical benefit—benefit supported by two controlled trials.”
-
Treatment with the new Alzheimer’s disease drug aducanumab requires considerable expertise and resource backup.
-
The panel recommendations need to be supplemented with further clinical discussion and clinical judgment.
Edward Susman, Contributing Writer, BreakingMED™
Cummings disclosed relationships with Acadia, Alkahest, AriBio, Avanir, Axsome, Behren Therapeutics, Biogen, Cassava, Cerecin, Cerevel, Cortexyme, EIP Pharma, Eisai, GemVax, Genentech, Green Valley, Grifols, Janssen, Jazz, Karuna, LSP, Merck, Novo Nordisk, Otsuka, ReMYND, Resverlogix, Roche, Signant Health, Sunovion, Suven, United Neuroscience, and Unlearn AI pharmaceutical and assessment companies. Cummings owns the copyright of the Neuropsychiatric Inventory.
Carrillo disclosed no commercial relationships.
Rabinovici reported grant support from Avid Radiopharmaceuticals, Inc., GE Healthcare, Genentech USA, Inc., and Life Molecular Imaging, as well as consultant agreements with EiSAI Inc., F. Hoffmann-La Rocher, GE Healthcare, Genentech, USA. Inc., and Johnson & Johnson Healthcare System, Inc.
Alexander reported consultant agreements with the FDA and OpturnRx. He is a principal in Monument Analytics.
Emerson resported a consultant agreement with Acadia Parmaceuticals, Inc.
Kesselheim reported grants from Arnold Ventures, and the FDA
Knopman reported grants from Biogen, Inc. Eli Lilly and Company, and Washington University in St. Louis School of Medicine.
Ovbiagele reported consultant agreements with AstraZeneca.
Cat ID: 130
Topic ID: 82,130,282,404,485,820,728,791,580,730,130,33,361,192,255,362,819,925,481,816


