It’s time to update the heart failure lexicon by acknowledging that data elements should not be differentiated between chronic heart failure and acute decompensated heart failure or inpatient versus outpatient, according to the American College of Cardiology/American Heart Association.
The last decade witnessed major advances in effective treatments for heart failure, from therapeutics such as angiotensin receptor-neprilysin inhibitor agents (ARNI) and sodium-glucose co-transporter 2 inhibitors (SGLT2-inhibitors) to implantable ventricular assist systems (VAS) and ventricular assist devices (VAD), but still lacking are specific data elements and definitions for accurate patient-level assessment of heart failure.
In addition to a lack of data, there is also a lack of uniformity, which can often limit the generalizability of findings.
The ACC/AHA are jumping in with both feet in attempting to remedy that knowledge gap with a 98 page statement (including 10 appendices) titled “Key Data Elements and Definitions for Measuring the Clinical Management and Outcomes of Patients With Chronic Heart Failure,” published online in the Journal of the American College of Cardiology.
The AHA data standards are designed to be “broadly applicable in various settings, including clinical programs such as HF clinics, transitions of care, clinical registries, clinical research, quality performance improvement initiatives, electronic health records and digital health information technology interoperability, public reporting programs, and education/ self-care.”
The document, which was produced by an eight-member writing committee led by Biykem Bozkurt, MD, PhD, of Baylor College of Medicine, and Ray E. Hershberger, MD, of The Ohio State Werner Medical Center, on behalf of the 27-member ACC/AHA Task Force on Clinical Data Standards, is also endorsed by the Heart Failure Society of America, the International Society for Heart and Lung Transplantation, and the Society of Thoracic Surgeons.
The writing committee pointed out a number of special considerations to keep in mind when reviewing the document: it does not attempt to differentiate “new onset incident versus prevalent cases,” nor does it differentiate “chronic HF versus acute decompensated HF; or for inpatients, outpatient, palliative care, or hospice status because HF is a chronic condition that is not an episodic event, and a patient can transition from one status to another through his/her life time,” they wrote.
The committee listed the goals for the statement:
- “To establish a consistent, interoperable, and universal clinical vocabulary as a foundation for clinical care and clinical research.
- “To facilitate the exchange of data across systems through harmonized, standardized definitions of key data elements.
- “To facilitate the further development of clinical registries, quality and performance improvement programs, outcomes evaluations, public reporting, and clinical research, including the comparison of results within and across these initiatives.”
Its release follows by just days a JAMA Cardiology publication of data from the National Heart Lung and Blood Institute’s Atherosclerosis Risk in Communities (ARIC) trial, which found measurement of left ventricular ejection fraction is not enough to accurately assess heart failure risk. An editorial that accompanied those results called the implications “profound” and noted that the calculus of heart failure prevention “must now incorporate important clinical variables, especially age, hypertension, obesity, and ischemic heart disease; biomarkers; and comprehensive measures of ventricular function that include strain. Even the definition of American College of Cardiology/American Heart Association stage A HF is worth reconsideration.”
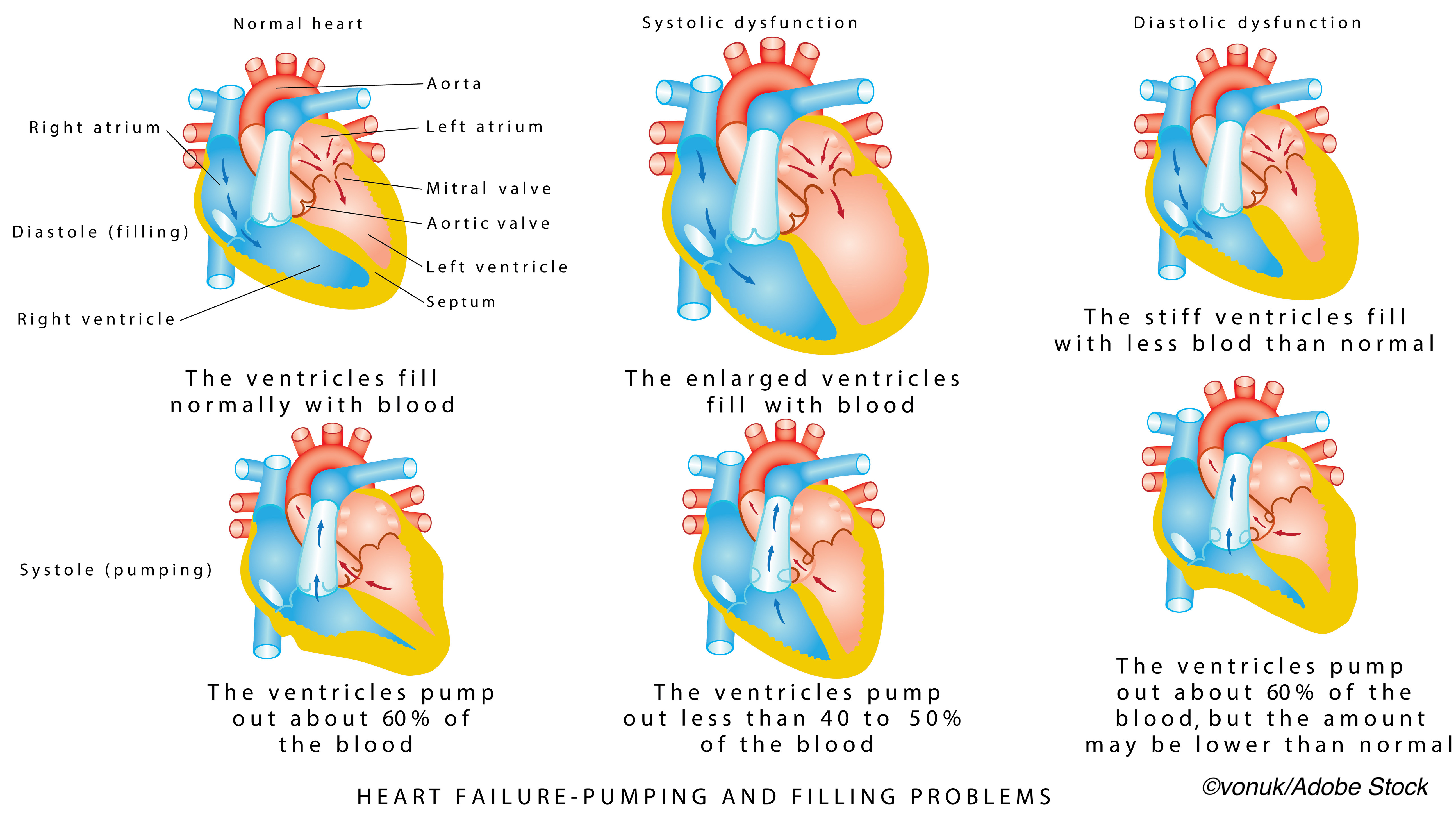
The ACC/AHA statement defines heart failure with reduced ejection fraction (HFrEF), also known as systolic HF or cardiomyopathy, as “HF in a patient with documented LVEF of ≤40%” and heart failure with preserved ejection fraction (HFpEF) “as a patient with documented LVEF of ≥50%,” while mid-range heart failure is defined as a patient with documented LVEF >40% and <50%.
Also included in HF stages are HF with recovered EF, which refers to HFrEF patients who have improved EF to ≥50%.
Other key data points:
- Duration of HF symptoms.
- Assessment of the cause of damage to the heart muscle, including “specific diagnoses such as cardiac amyloidosis and peripartum cardiomyopathy.”
- Collection of data echocardiogram, cardiac MRI, and cardiopulmonary exercise testing.
- Data elements for invasive therapeutic procedures (device therapies and mechanical circulatory support devices).
The statement also includes pharmacological treatments “with new classes of medications updated, and new data elements for new classes of medications,” as well as data elements for patient education and patient-reported outcomes.
-
Be aware that the language in this 2021 update of key data points and definitions does not differentiate between chronic or acute heart failure, inpatient versus outpatient, or whether patients are receiving palliative care. Thus, the data elements apply to the full range of care provided to patients with heart failure and are intended to be useful for all care settings.
-
The ACC/AHA writing committee contends that health failure data standards are more critical now for clinical providers, investigators, administrators, health care services and institutions, regulators, legislators, and payers because of the growing burden of heart failure and increasing focus on performance measures.
Peggy Peck, Editor-in-Chief, BreakingMED™
Boskurt reported no relevant relationships with industry.
Hershberger reported no relevant relationships with industry.
Cat ID: 3
Topic ID: 74,3,730,3,914,127,192,925


