Does adding metformin to chemoradiotherapy in patients with locally advanced NSCLC improve survival rates? This article details results from two large clinical trials—OCOG-Almera and NRG-LU001—and was originally published on July 29, 2021 and is included in our year-end review of BreakingMED stories. Click here to see the original article and obtain CME/CE credit for the activity.
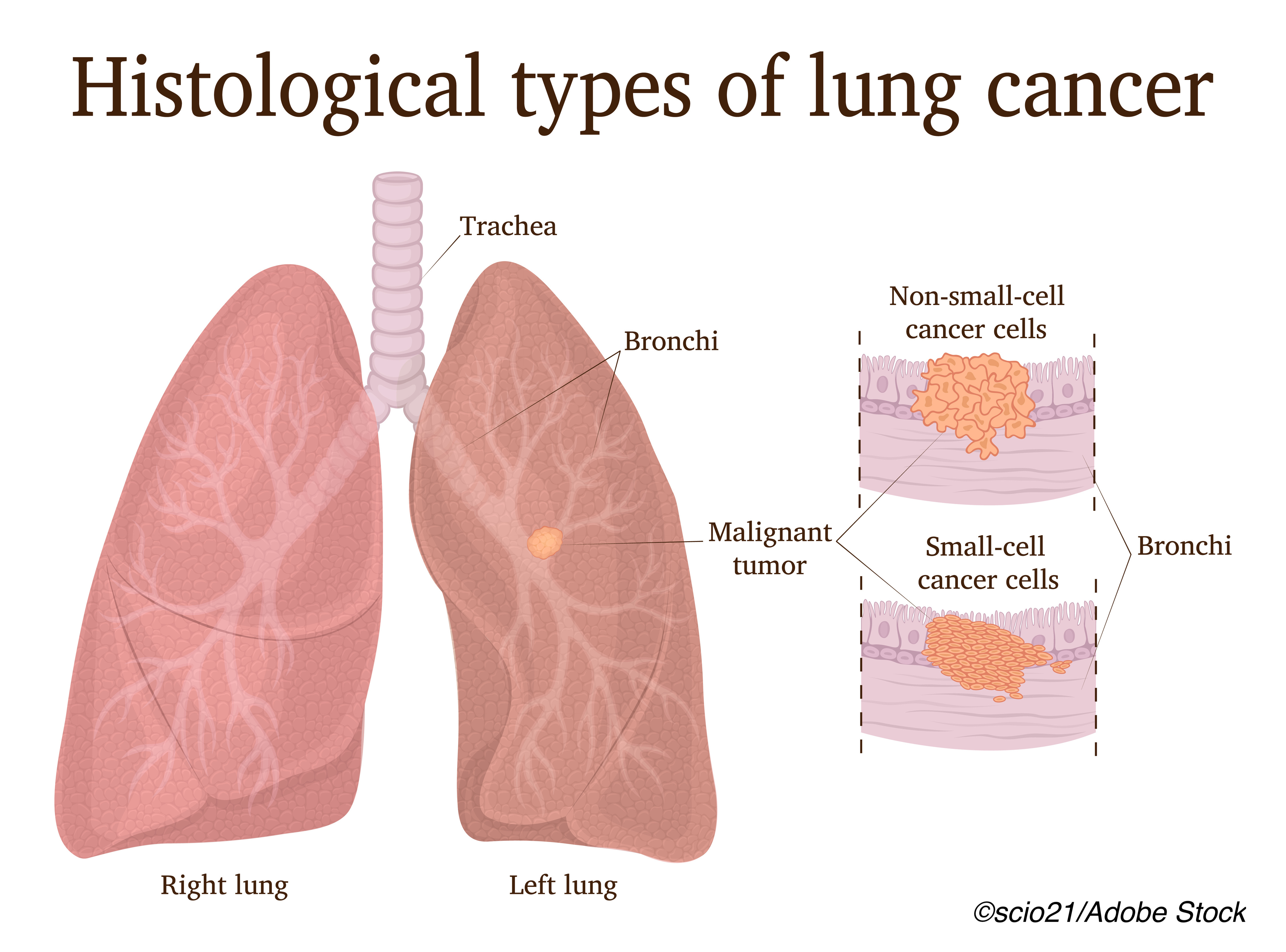
Adding metformin to chemoradiotherapy in patients with locally-advanced non–small cell lung cancer (LA-NSCLC) did not improve survival, according to results from two large clinical trials, OCOG-ALMERA and NRG-LU001. And, in the former study, the addition of metformin caused greater toxicity compared with chemoradiotherapy alone. Both studies were published in JAMA Oncology.
Theodoros Tsakiridis, MD, PhD, of the Juravinski Cancer Center, McMaster University, Ontario, Canada, and colleagues, who conducted the OCOG-ALMERA study, detailed the rationale behind the use of metformin—currently approved only for the treatment of type 2 diabetes—in patients with NSCLC.
“Metformin, the most widely used type 2 diabetes agent, is proposed to suppress tumor growth through metabolic stress caused by inhibition of complex I of the mitochondria oxidative phosphorylation chain. In preclinical NSCLC models, metformin activated AMPK, induced p53, suppressed mammalian target of rapamycin and tumor growth, and enhanced tumor response to radiotherapy and chemotherapy. These findings are supported by retrospective clinical evidence of improved survival in LA-NSCLC among patients with diabetes treated with metformin,” they wrote.
For this multicenter, phase II, randomized study, Tsakiridis and colleagues stratified 54 patients (mean age: 65.6 years; 55.6% women) with unresected LA-NSCLC without diabetes according to cancer stage (IIIA vs IIIB). Patients were then randomized to platinum-based chemotherapy with chest radiotherapy (60-63 Gy) with or without consolidation chemotherapy, or the same regimen plus metformin (2,000 mg/d) during chemotherapy and for an additional 12 months after chemo. The trial was stopped early due to slow accrual of patients.
Within 1 year, treatment failure occurred in significantly more patients treated with the addition of metformin compared with controls (55.6% versus 42.9%, respectively; P=0.05). At this same time point, progression-free survival (PFS) was also significantly worse in patients treated with metformin (34.8% versus 63.0%; HR: 2.42; 95% CI: 1.14-5.10).
Finally, overall survival (OS) rates were also significantly worse in patients treated with metformin compared with controls (47.4% versus 85.2%, respectively; HR: 3.80; 95% CI: 1.49-9.73). One or more Grade 3 or higher adverse events were reported by 53.8% of patients treated with metformin compared with only 25.0% of control patients.
Researchers of the NRG-LU001 open-label, phase 2, randomized trial, led by Heath Skinner, MD, PhD, had the same idea.
“Metformin has been studied extensively for its potential antineoplastic effects. This research was prompted by epidemiologic studies showing a reduced incidence of cancer and retrospective case studies showing improved outcomes in patients taking metformin. Preclinical data suggested a wide range of antineoplastic effects of metformin, mediated by its ability to stimulate adenosine monophosphate–activated kinase and inhibit the mammalian target of rapamycin pathway. Indeed, metformin monotherapy exhibits cytostatic and cytotoxic effects both in vivo and in,” they wrote.
“Moreover, individual combinations of metformin and platinum or radiation have shown at least additive effects in multiple preclinical models, including NSCLC. These clinical and preclinical data, coupled with the well-described safety profile and affordability of metformin, led to NRG-LU001,” they added.
Skinner and colleagues—included Tsakiridis from OCOG-ALMERA—randomized 167 patients (median age: 64 years; 58.1% men; 82.0% White) with stage III NSCLC to treatment with chemoradiation alone or chemoradiation with metformin. Patients were followed for a median of 27.7 months.
One-year PFS rates were lower in patients treated with metformin compared with chemoradiation alone (51.3% versus 60.4%, respectively (HR: 1.15; 95% CI: 0.77-1.73; P=0.24). One-year OS was similar between the two groups (80.8% versus 80.2%). No significant differences were seen in either local-regional recurrence or distant metastasis at 1 or 2 years.
Upon multivariate analysis, Skinner and fellow researchers found that the only factor significantly associated with PFS was clinical stage (HR: 1.79; 95% CI: 1.19-2.69; P=0.005). Finally, they found no significant differences in adverse events between the two groups.
Nevertheless, some are still hopeful that metformin may still play a role in the treatment of patients with inoperable LA-NSCLC.
“Despite the negative results of both studies, invaluable information for the subsequent design of future trials could be extracted. There might yet be a role for metformin in selected patients with NSCLC patients: KRAS/LKB1-mutated tumors or tumors with elevated fluorodeoxyglucose metabolism. Future trial designs should incorporate continuous assessment of metabolic parameters, including aerobic and nonaerobic glycolysis, comprehensive longitudinal functional imaging response assessment, and biomarker analyses,” wrote Chukwuka Eze, MD, and colleagues in an accompanying editorial.
OCOG-ALMERA study limitations include the lack of double-blinding, placebo control, and limited accrual. Limitations of the NRG-LU001 study included issues with patient compliance and tolerance of metformin and the lack of placebo control due to cost restrictions.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
The OCOG-ALMERA study was funded by a grant from the Canadian Institutes of Health Research. The Ontario Clinical Oncology Group (OCOG) assumed the role of the sponsor of this trial.
Tsakiridis reported receiving a grant from Sanofi Canada for prostate cancer research outside the submitted work, and grants from the Canadian Institutes of Health Research for metformin-related clinical trials; and fees from AstraZeneca, Sanofi, and AbbVie outside the submitted work.
The NRG-LU001 study was supported by grants from the National Cancer Institute.
Skinner reported receiving research funding from the National Cancer Institute and National Institute of Dental and Craniofacial Research outside the submitted work and has previously received a grant from the National Cancer Institute for a separate metformin-related clinical trial.
Eze reported no disclosures.
Cat ID: 24
Topic ID: 78,24,730,24,192,65,925,480,482,96


