1. Atezolizumab plus capecitabine + bevacizumab performed marginally better with regards to progression free survival in patients with metastatic colorectal cancer, but did not demonstrate meaningful clinical difference.
2. Patients with microsatellite stability, no liver metastasis and proficient mismatch repair were more likely to benefit from dual inhibition of several targeted pathways.
Level of Evidence: 1 (Excellent)
Study Rundown: In recent years, the focus of systemic treatment of metastatic colorectal cancer has shifted to include combinations of targeted therapies (i.e., programmed cell death ligand 1, anti-programmed cell death 1) with improved outcomes. However, these therapies are more likely to benefit a select group of patients based on specific tumor characteristics of microsatellite instability and mismatch repair dysfunction. Preclinical research has demonstrated that patients with proficient mismatch repair (pMMR) and microsatellite stability (MSS) may derive benefit from the combination of a vascular endothelial growth factor inhibitor with inhibition of the programmed cell death axis. The present Phase 2, randomized trial sought to evaluate whether atezolizumab in combination with capecitabine + bevacizumab (ABC) improved progression-free survival (PFS) compared to capecitabine + bevacizumab (BC) alone. 128 patients contributed to the analysis, with 82 in the intervention group and 46 in the control group. 110 patients (89.4%) had MSS/pMMR disease, the proportion of which was balanced at baseline between the two groups. Median PFS in the interventional group was 4.4 months from randomization, and was 3.6 months in the control group; this difference was not statistically significant. The estimated PFS at 1 year was 15.2% in the intervention group and 6.9% in the control group. Median overall survival was similar, at 10.3 months in the ABC group and 10.2 months in the BC group. Subgroup analysis revealed that patients without metastases to the liver had higher response rates to ABC therapy in general, although statistical significance was not reached in comparison of overall survival. Rates of adverse events were also similar between the two study groups. This randomized, Phase 2 trial demonstrated that the addition of atezolizumab to standard BC therapy in the treatment of refractory, metastatic colorectal cancer did not prolong progression free survival or overall survival to a substantial degree. A subgroup of patients without liver metastases, whose tumors were MSS and pMMR+ may have a higher likelihood of responding to ABC therapy, although this relationship requires further investigation. Strengths of this work include the randomized design as well as large sample size, which adequately powered this trial to detect significant differences in tumor response. A major limitation was the lack of standardized control of certain inclusion criteria (i.e., microsatellite instability status, imaging review) between sites.
Click here to read this study in JAMA
Relevant Reading: Selecting treatment options in refractory metastatic colorectal cancer
In-Depth [randomized controlled trial]: The methodology of the present study (the BACCI trial) was a phase II, double-blinded, placebo-controlled, multicentered, randomized design. Patients were enrolled between September 25, 2017 and June 28, 2018. Eligible patients were adults with histology-confirmed metastatic colorectal cancer who had experienced disease progression or treatment intolerance while on one of the following therapies: fluorouracil, capecitabine, oxaliplatin, irinotecan, bevacizumab and anti-epidermal growth factor. Patients must have never previously been treated with PD-1/PD-L1 inhibitors. Patients were randomized in a 2:1 fashion to receive either the ABC or the BC regimen using a computerized system. Both patients and members of the study team were blinded to treatment allocation. Outcomes were assessed after every 3 cycles (each cycle was 21 days). Median PFS was 4.4 months in the intervention group (95% confidence interval [CI] 4.1-6.4) and 3.6 months in the control group (95% CI 2.2-6.2). The hazard ratio comparing PFS was 0.75 (95% CI 0.52-1.09). Estimated rates of PFS at 12 months were 15.2% in the intervention group (95% CI 9.1-25.6%) and 6.9% (95% CI 2.3-20.5%) in the control group. Median overall survival was 10.3 months in the ABC group vs 10.2 months in the BC group ([ABC 95% CI, 8.3-15.2 months] vs [BC 95% CI, 8.5-16.6 months]. The hazard ratio for overall survival was 0.96 [95% CI, 0.63-1.45]. An additional analysis of patients without liver metastasis found that this subgroup tended to have a better response rate to the ABC therapy (23.1% response rate) compared to the patients with liver metastases who had a 5.3% response rate to ABC treatment (p=0.04). In the trial’s safety analysis, 80 patients reported adverse events rated Grade 3 or higher, most commonly: hypertension, abdominal pain, diarrhea, hand-foot syndrome and fatigue.
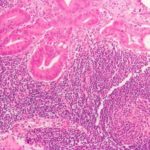
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.