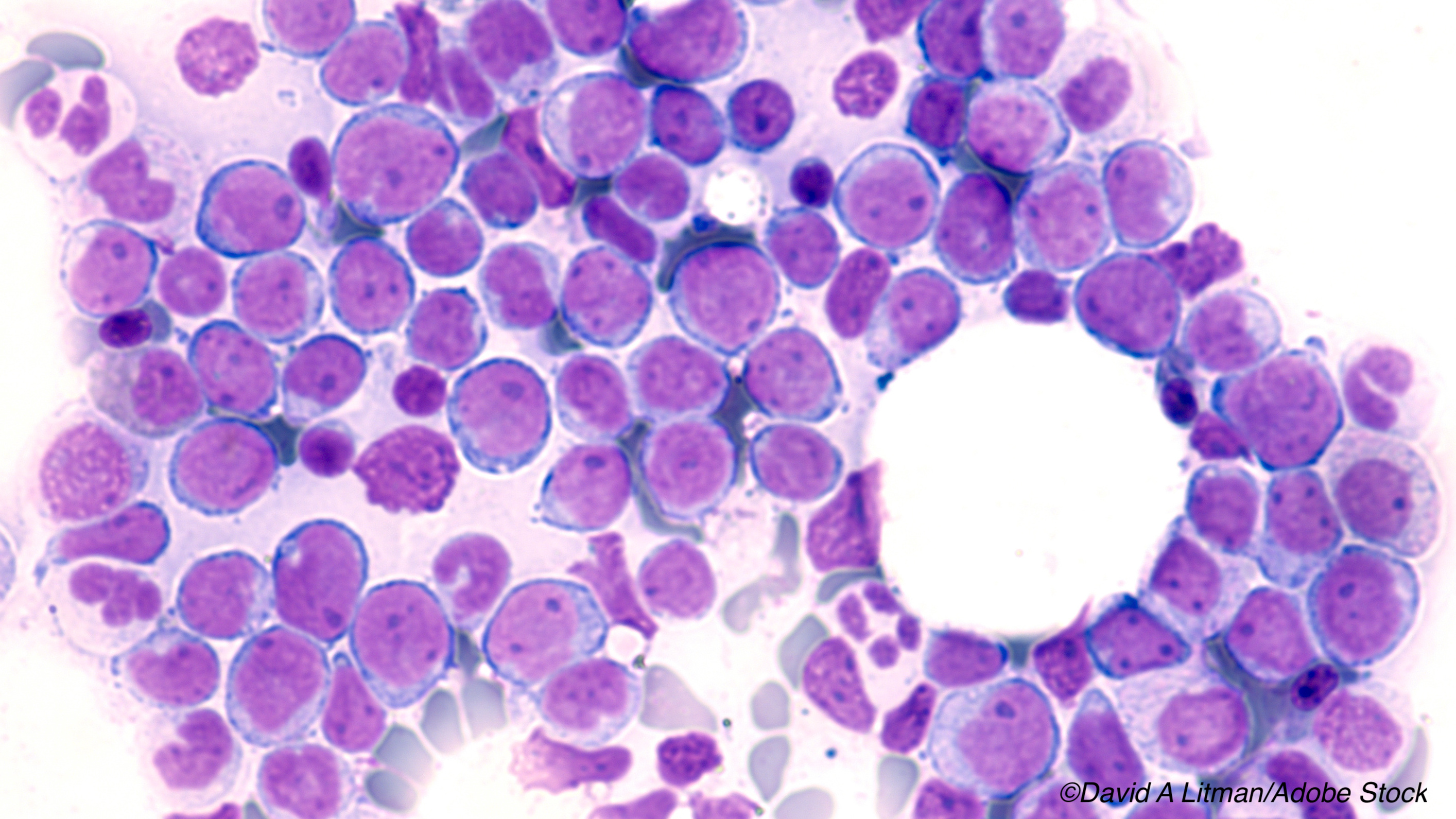
 In patients with acute myeloid leukemia (AML), achieving measurable residual disease (MRD) negativity is significantly associated with superior long-term and disease-free survival (DFS), according to results of a large systematic review and meta-analysis published in JAMA Oncology. Researchers concluded that assessing MRD status in AML patients should guide both clinical decision-making and upcoming clinical trials on the efficacy of new therapies for AML.
In patients with acute myeloid leukemia (AML), achieving measurable residual disease (MRD) negativity is significantly associated with superior long-term and disease-free survival (DFS), according to results of a large systematic review and meta-analysis published in JAMA Oncology. Researchers concluded that assessing MRD status in AML patients should guide both clinical decision-making and upcoming clinical trials on the efficacy of new therapies for AML.
“Although many publications have suggested substantial clinical value of MRD assessment in AML, the optimal use of MRD information to risk stratify patients and inform clinical decision-making has been limited in part by the heterogeneity of these reports,” wrote lead author Nicholas J. Short, MD, of the University of Texas MD Anderson Cancer Center, Houston, and fellow researchers.
“To use MRD information to guide clinical decision-making in AML and support its use as a meaningful clinical end point, it is necessary to understand the strength of the association of MRD with survival outcomes and the consistency of this association across patient-related, disease-related, and methodologic variables,” they explained.
To address this, Short and colleagues searched PubMed, Embase, and MEDLINE for all clinical trials that assessed disease free survival (DFS) or overall survival (OS) by MRD status in patients with AML published between January 1, 2000, and October 1, 2018. In all, they found 81 studies in a total of 11,151 patients.
In all AML patients, the average hazard ratio (HR) for achieving MRD negativity was 0.36 (95% Bayesian credible interval [CrI]: 0.33-0.39) for OS and 0.37 (95% CrI: 0.34-0.40) for DFS. In patients with negative MRD, the estimated 5-year DFS was 64% (95% CrI: 59%-70%), and in those without MRD-negativity, 25% (95% CrI: 20%-32%). Corresponding 5-year OS rates were 68% (95% CrI: 63%-73%) and 34% (95% CrI: 28%-40%), respectively.
The difference in 5-year restricted mean survival times was 15.37 months (95% CrI: 13.58-17.19 months) for OS, and 19.61 months (95% CrI: 17.33-21.92 months) for DFS.
Similar results were seen upon univariate analysis of the different subgroups of patients, with MRD-negativity associated with superior DFS and OS regardless of age (adult or pediatric), time of MRD assessment (during induction or consolidation, or after consolidation), AML subgroup (core-binding factor [CBF] or non-CBF), or source of specimen (bone marrow or peripheral blood).
Upon subgroup analysis, associations between MRD and survival outcomes were more significant for CBF AML compared with non-CBF AML (OS posterior probability: 0.999; DFS posterior probability: 0.997). In addition, peripheral blood assessment of MRD was superior to bone marrow assessments in regard to distinguishing MRD positivity and negativity (OS posterior probability: 0.918; DFS posterior probability: 0.999).
MRD status was assessed in the various clinical trials with multiparameter flow cytometry, polymerase chain reaction (PCR), PCR Wilms tumor 1, next-generation sequencing, or cytogenetics/in situ hybridization. In all subgroups of patients except those with MRD assessed via cytogenetics or fluorescent in situ hybridization, the association of MRD negativity with DFS and OS was significant. The association between MRD and differences in OS and DFS using cytogenetics/FISH was non-significant (average HR for OS: 0.77; 95% CrI: 0.39-1.56 and average HR for DFS: 0.65; 95% CrI: 0.34-1.23).
“The lack of significant association of cytogenetics/FISH with DFS and OS may be explained in part because only 2 studies using this method were included in this analysis (527 patients total) and because this MRD detection method has the lowest sensitivity among those considered,” explained Short and fellow researchers.
“This meta-analysis of 81 publications suggests that MRD status has prognostic importance in AML and may be a valid surrogate marker for both DFS and OS in AML clinical trials. The magnitude of benefit associated with achieving MRD negativity was substantial, corresponding to a 64% reduction in the risk of death for MRD-negative patients. The results of this meta-analysis thus provide quantitative support for consensus guidelines that consider achievement of complete remission without MRD as the optimal response in AML,” they concluded.
Authors of an accompanying editorial, Deepa Jeyakumar, MD, and Susan O’Brien, MD, both of the University of California-Irvine, Orange, CA, agreed.
“[MRD] positivity vs negativity appeared to result in significant differences in [DFS] as well as [OS] in patients with AML. These data emphasize the need to incorporate MRD analysis into the care of patients with AML,” they wrote.
Jeyakumar and O’Brien also stressed the applicability of these results in the development of new therapeutic options for AML, which are sorely needed.
“[I]t may be beneficial to use MRD negativity as a surrogate end point for clinical trials in AML to facilitate drug development. Given that the standard of care therapy for AML of ’3+7’ has not changed in over 40 years and yet cures only a minority of adults with AML, more rapid drug development of therapies for AML is needed. A lesson learned from the Ratify trial is that it took over a decade from study conception to US Food and Drug Administration approval of midostaurin based on using overall survival as a primary end point. Surrogate end points may aid in getting effective therapies to patients expeditiously while still confirming the benefit of these agents with an assessment of overall survival,” they concluded.
-
Measurable residual disease (MRD)-negativity in patients with acute myeloid leukemia (AML) is associated with better disease-free survival (DFS) and overall survival (OS), and was consistent across all ages, subtypes of AML, time of MRD assessment, source of specimen, and MRD detection methods used.
-
MRD status may be an important endpoint in clinical decision-making and finding new therapeutic options for these patients.
E.C. Meszaros, Contributing Writer, BreakingMED™
This study was supported by MD Anderson Cancer Center and the Intramural Research Program of the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Short reported support from the K12 Paul Calabresi Clinical Oncology Scholar Award and the American Society of Hematology Junior Faculty Scholar Award in Clinical Research.
Jeyakumar and O’Brien reported no conflicts of interest.
Cat ID: 118
Topic ID: 78,118,118,466,935,192,925


