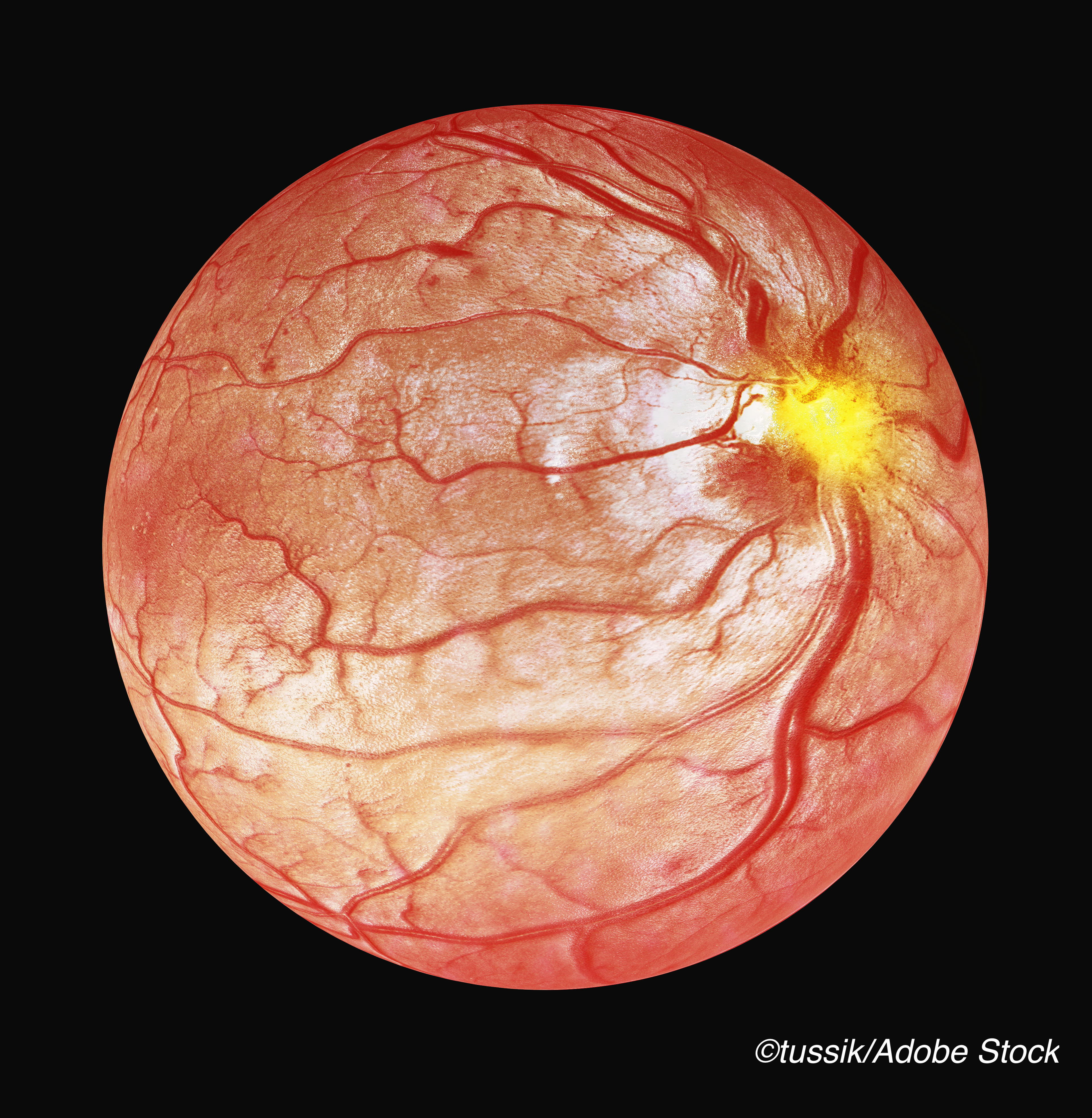
In the future, automated optical coherence tomography (OCT) measurements of central macular fluid volume (CMFV) may give clinicians more accuracy in diagnosing diabetic macular edema (DME), the predominant cause of visual impairment in patients with diabetes, according to a study published in JAMA Ophthalmology. But, until OCT and OCT angiography (OCTA) become more economical, these results hold only promise, rather than wide-spread applicability.
“In recent years, optical coherence tomography (OCT) has supplanted stereoscopic fundus photography and fundus biomicroscopy for the diagnosis of DME. Optical coherence tomography detects key, clinically relevant features in DME, including macular thickening and intraretinal and subretinal fluid. Optical coherence tomography has the potential to improve DME screening, as reported previously,” wrote Qi Sheng You, MD, PhD, of the Casey Eye Institute, Oregon Health & Science University, Portland, and fellow researchers.
For their cross-sectional, observational study, You and colleagues included one eye each from 215 patients (mean age: 59.6 years; 54.4% women) enrolled in two studies being conducted at the Casey Eye Institute. Patients were aged 18 to 85 years and had either type 1 diabetes for more than five years or type 2 diabetes for any length of time.
All patients underwent comprehensive medical exams, 6 x 6-mm macular structural OCT horizontal raster scans (which also measured mean central subfield thickness [CST] within the central fovea), and 6 x 6-mm macular OCT angiography volumetric scans. The latter were reviewed by two retinal specialists, who diagnosed DME in patients with evidence of intraretinal or subretinal fluid. Any discrepancies were arbitrated by a third retinal specialist. For patients with fluid within the 1-mm central fovea, DME was logged as center involved.
You and fellow researchers then used a deep learning algorithm to automatically quantify fluid volumes from the 6 x 6-mm angiography volumetric scans and within the central foveas (CMFV).
In all, 63.3% of eyes (n=136) were diagnosed with DME via structural OCT raster scans, 93 of which were center-involved. Although DME was present at any DR stage, it increased as DR severity increased.
The area under the receiver operating characteristic curve (AUROC), one of the primary outcomes, was larger for CMFV for the diagnosis of center-involved DME compared with the AUROC of CST (0.907 vs 0.832, respectively; P=0.02).
At a set specificity of 95%, the sensitivity of CMFV for detecting center-involved DME was higher than that of CST (78.5% vs 53.8%; P=0.002), as was its sensitivity for detection of center-involved DME was 78.5% for CMFV versus 53.8% for CST (P=0.002).
DME cases that were center-involved and not detected via CST but detected by CMFV were associated with a thinner CST (290.8 vs 369.4 μm; P˂0.001), a higher proportion of previous macular laser treatment (39.3% vs 18.5%; P=0.03), and female sex (71.4% vs 47.7%; P=0.04).
In an accompanying editorial, Aaron Y. Lee, MD, MSCI, and Amy Yuan, MD, both of the University of Washington, Seattle, commented on the increasing promise of artificial intelligence (AI) in the field of ophthalmology, with important AI research in glaucoma, age-related macular degeneration, and retinopathy. Studies of AI as applied to DR, however, are lacking.
“At a glance, the hypothesis that a direct measure of fluid (with total volume of cystoid changes) is more specific for the diagnosis of DME than an indirect measure (the arithmetic mean of internal limiting membrane-to-retinal pigment epithelium segmentation within 1 mm of the fovea) would seem to be self-evident, although its value in place of, or in addition to, central subfield thickness measured by OCT scan has not yet been proven, to our knowledge,” they noted.
“However, the technical challenge of accurate and efficient segmentation of intraretinal cystoid changes to compute volume on OCT scans has historically been an impractical task,” they added.
According to Lee and Yuan, while these findings on the applicability of AI to ophthalmology are hopeful, they will not come to fruition until “OCT and OCTA become economical enough for routine DR screening.”
They concluded: “Until then, color fundus photography will likely continue to be the most practical imaging data for deep learning algorithms to tackle in addressing the quandary of efficient screening. A more immediate application of fully automated volumetric retinal fluid quantification from OCT and OCTA scans as described might be its use as a biomarker to monitor disease progression and response to therapy for any exudative retinal disease.”
Study limitations include its cross-sectional design, the possibility that CMFV may have been missed in eyes with a low signal strength index, and the limited generalizability of the algorithm due to its requirement for dense OCTA volumetric scans for accurate measurement of fluid volume and to the inclusion and exclusion criteria.
-
Automated OCT measurements of central macular fluid volume (CMFV) may improve diagnostic accuracy for diabetic macular edema (DME).
-
CMFV may be a more accurate biomarker for DME than central subfield thickness of the central fovea.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was supported by grants from the National Institutes of Health, an unrestricted departmental funding grant, and the William & Mary Greve Special Scholar Award from Research to Prevent Blindness.
You reported no conflicts of interest.
Lee reported receiving grants from the National Eye Institute/ National Institutes of Health during the conduct of the study; grants from Santen, Regeneron, Carl Zeiss Meditec, and Novartis; personal fees from the US Food and Drug Administration; personal fees from Genentech, Gyroscope, Topcon, and Verana Health; and nonfinancial support from Microsoft outside the submitted work. No other disclosures were reported.
Cat ID: 240
Topic ID: 92,240,730,12,669,918,925,240


