Bariatric surgery patients with comorbidities including diabetes, hypertension, and hyperlipidemia who undergo gastric bypass may be less likely to require obesity-related medications than those who undergo sleeve gastrectomy, according to a recent study published in JAMA Surgery.
Researchers found that, compared with sleeve gastrectomy, gastric bypass surgery was associated with both slightly higher incidence of medication discontinuation after surgery and slightly lower incidence of medication re-initiation. Differences between the two procedures were marginal, however. In addition, the highest rates of discontinuation and lowest medication restart rates occurred in patients with diabetes.
“Although gastric bypass may be associated with a slightly higher rate of diabetes remission, sleeve gastrectomy was also found in multiple studies to have durable diabetes remission. Other studies have suggested that gastric bypass may be associated with superior hypertension and hyperlipidemia resolution; however, these studies were limited by their small sample size. Even less is known regarding comparative outcomes in Medicare beneficiaries among whom obesity and bariatric surgery are increasingly common, but evidence to inform decision-making is lacking. Informed surgical decision-making requires understanding the differences in obesity-related outcomes of these procedures,” wrote Ryan Howard, MD, of the University of Michigan, Ann Arbor, and co-authors.
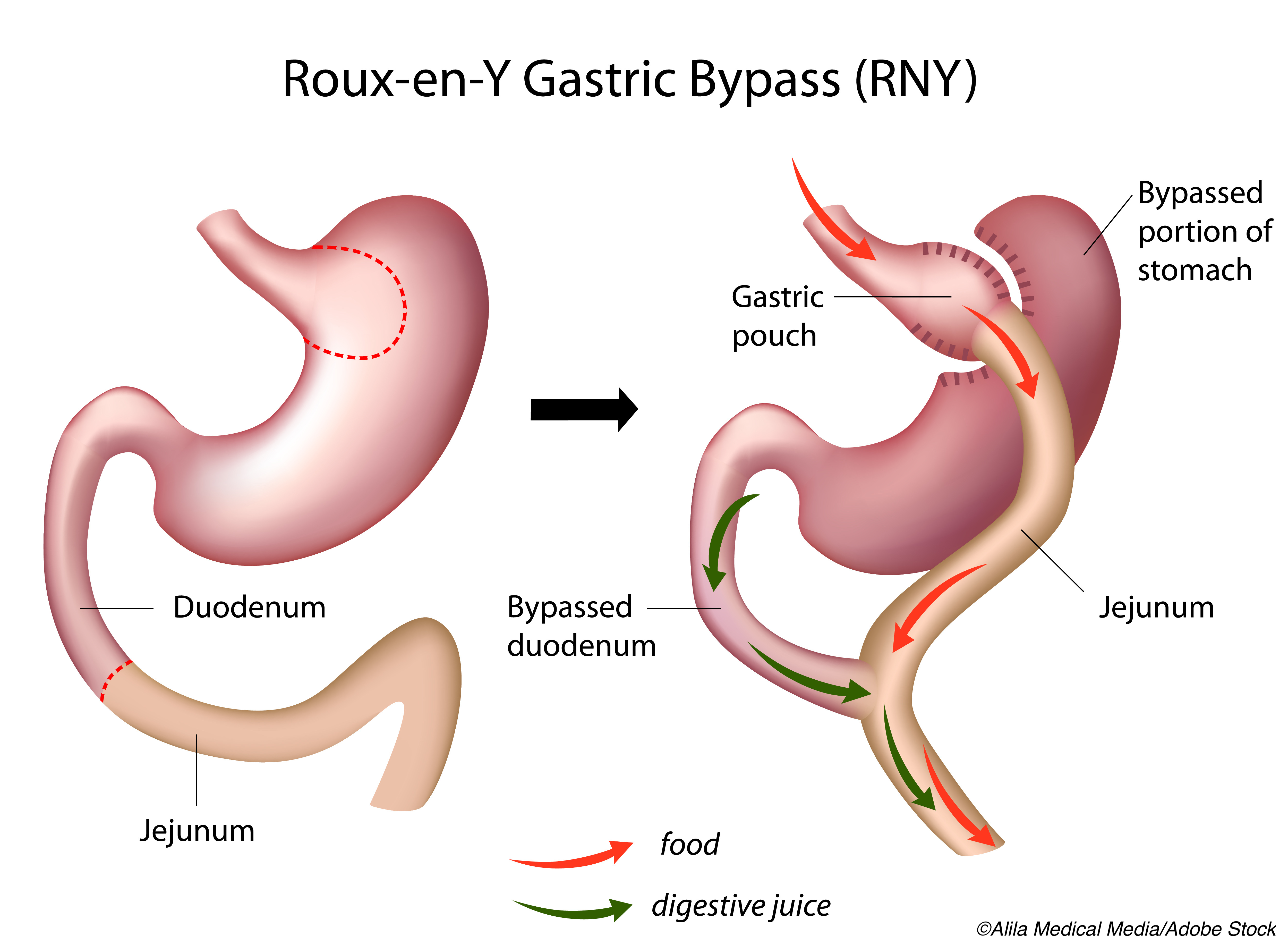
Thus, to determine the long-term comparative efficacy of sleeve gastrectomy and gastric bypass procedures, they included 95,405 Medicare beneficiaries (mean age: 56.6 years; 74.8% women) who had undergone laparoscopic sleeve gastrectomy or Roux-en-Y gastric bypass, the two most common surgical procedures for severe obesity. All patients had received medications for diabetes, hypertension, or hyperlipidemia in the 6 months preceding surgery.
The primary outcome was the discontinuation of medications for any of these three conditions for any reason. Researchers also determined the adjusted incidence of medication re-initiation up to 5 years after initial discontinuation.
Upon analysis, researchers found that gastric bypass was associated with a slightly higher 5-year cumulative incidence of medication discontinuation in patients with diabetes medication use and diagnosis at the time of surgery, compared with sleeve gastrectomy (74.7% vs 72.0%, respectively), patients using antihypertensive medications (53.3% vs 49.4%), and those using lipid-lowering medications (64.6% vs 61.2%).
In patients who discontinued any medication, gastric bypass was also associated with a lower incidence of restarting those medications compared with sleeve gastrectomy up to 5 years after they were discontinued, as follows:
- Patients discontinuing diabetes medications: 30.4% vs 35.6%, respectively;
- Patients discontinuing antihypertensive medications: 67.2% vs 70.6%; and
- Patients discontinuing lipid-lowering medications: 46.2% vs 52.5%.
“This study by Howard et al is unique in that its population was large (nearly 100 000 patients) and older by about 10 years compared with the population of much of the studies in bariatric surgery literature. Therefore, the finding that gastric bypass surgery was associated with a slightly higher chance of medication discontinuation and a lower chance of later medication restart meant that, for this broader group of patients, a gastric bypass procedure may have a bigger advantage over a gastric sleeve procedure for the treatment of diabetes, hypertension, and dyslipidemia,” wrote Anita P. Courcoulas, MD, MPH, and Bestoun H. Ahmed, MD, both of the University of Pittsburgh Medical Center, in their invited commentary.
They did note the important limitations to be considered, including the use of administrative claims data, a lack of data on actual medication use as prescribed, and reasons for medication discontinuation other than resolution of the comorbid condition.
Other study limitations cited by Howard and co-authors include the limited generalizability of results due to the use of Medicare claims data; the reliance of researchers on an arbitrary window of time during which no medication claims were recorded; the possibility of residual bias due to differences in mortality, unenrollment from Medicare, and medication compliance; and the large sample size.
Despite these limitations, Courcoulas and Ahmed noted, these results are important for both clinicians and patients in choosing bariatric procedures.
“Howard et al focused completely on medications as an end point for comorbid health change, which is something that is important to many patients who seek bariatric and metabolic surgery not only to achieve durable weight loss but also to relieve the burden of using multiple medications. The measures used in this study may not be perfect surrogates, but the findings do help to inform prospective patients and their physicians about what they can relatively expect after undergoing either of the 2 most common bariatric surgical procedures,” they concluded.
-
Although both gastric bypass and sleeve gastrectomy brought about high medication discontinuation rates for comorbidities—including diabetes, hypertension, and hyperlipidemia—gastric bypass had a slightly higher rate of discontinuation and a slightly lower rate of medication restart.
-
Patients with diabetes demonstrated the highest medication discontinuation rates and lowest medication restart rates.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Howard was supported by grants from Blue Cross Blue Shield of Michigan Foundation and the NIDDK outside the submitted work.
Courcoulas reported receiving grants from National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, and Patient-Centered Outcomes Research Institute and grants from Allurion Inc outside the submitted work.
Ahmed reported no disclosures.
Cat ID: 12
Topic ID: 76,12,730,4,446,6,12,795,518,669,917,925,159


