 A systematic review of studies on adhesive capsulitis — also known as frozen shoulder — found that patients consistently had better outcomes when offered an intra-articular (IA) corticosteroid early in the course of treatment.
A systematic review of studies on adhesive capsulitis — also known as frozen shoulder — found that patients consistently had better outcomes when offered an intra-articular (IA) corticosteroid early in the course of treatment.
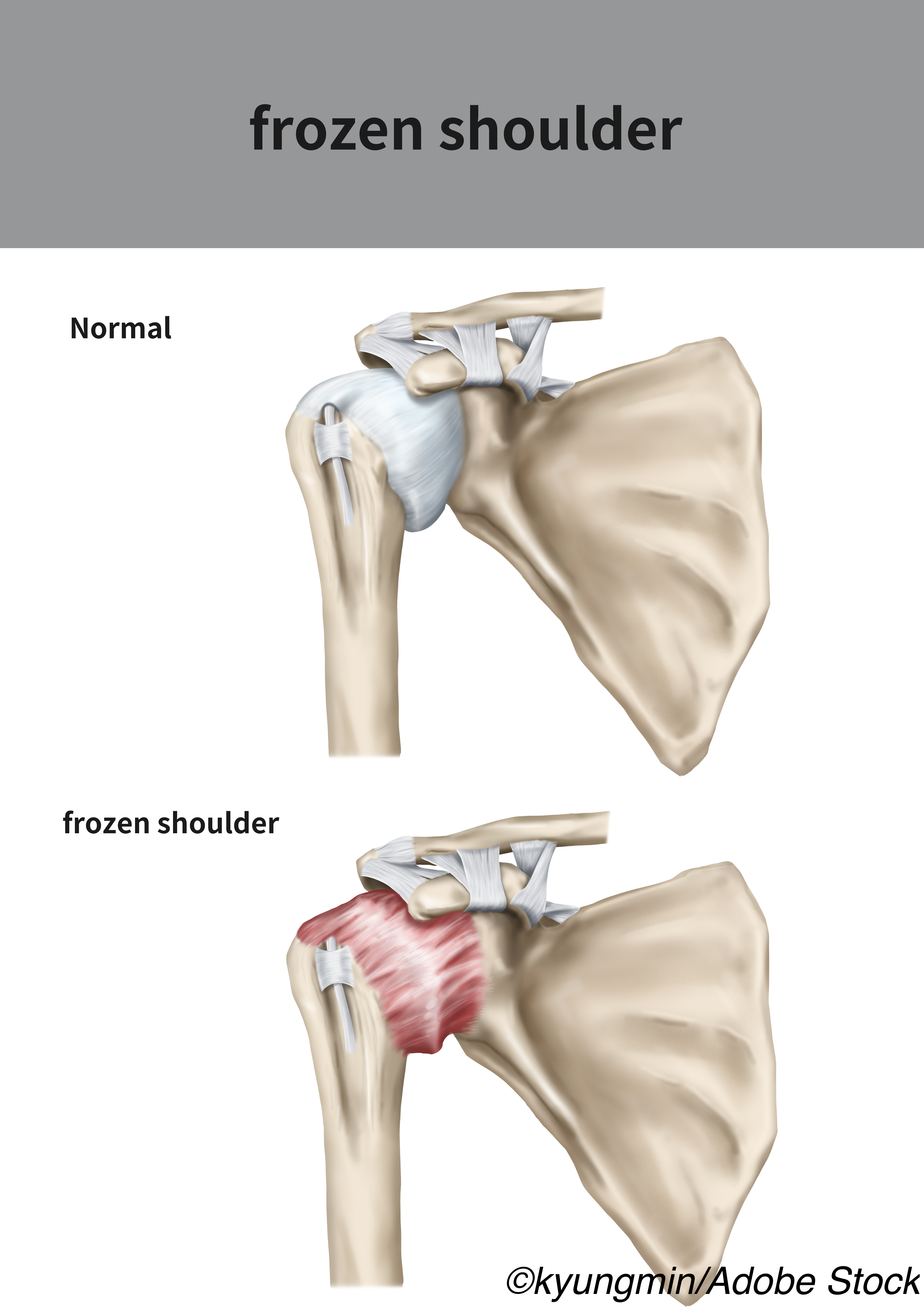
Frozen shoulder, a fibroproliferative tissue fibrosis that causes progressive loss of glenohumeral movement and shoulder pain, is a common shoulder concern, Neal L. Millar, MD, PhD, of the Institute of Infection, Immunity, and Inflammation at the College of Medicine in the Veterinary and Life Sciences University of Glasgow in Glasgow, U.K., and colleagues explained — however, while immunobiological advances in other diseases have helped clarify the pathophysiology of the condition, its molecular mechanisms are poorly understood, and there are currently no firm recommendations for clinical practice.
To help determine the best available treatment options for patients with frozen shoulder and inform guidelines for disease treatment, Millar and colleagues conducted a systemic review of 65 studies assessing various treatment strategies for frozen shoulder and performed a pairwise meta-analysis to compare each intervention: IA corticosteroid, physiotherapy, IA corticosteroid plus physiotherapy, subacromial corticosteroid, arthrographic distension plus IA corticosteroid, acupuncture plus physiotherapy, or no treatment/placebo.
“Based on the available evidence, it appears that the use of an IA corticosteroid for patients with frozen shoulder of duration less than 1 year is associated with greater benefits compared with all other interventions, and its benefits may last as long as 6 months,” they reported in JAMA Network Open. “This has important treatment ramifications for the general and specialist musculoskeletal practitioner, providing them with an accessible, cost-effective, and evidence-based treatment to supplement exercise regimes, which we anticipate will inform national guidelines on frozen shoulder treatments moving forward.”
For their analysis, Millar and colleagues searched Medline, EMBASE, Scopus, and CINHAL for studies assessing treatment strategies for frozen shoulder in February 2020. “From a total of 73,299 articles that were initially identified, after exclusion of duplicate and noneligible articles, title and abstract screening, and the addition of missed studies identified subsequently, 65 studies were found to fulfill the eligibility criteria,” the study authors explained.
Outcomes were divided into short-term (≤12 weeks), mid-term (>2 weeks to ≤12 months), and long-term (>12 months) follow-up, and when pain results were reported in different settings — at rest, at night, with activity, etc. — only pain at rest was used in the review’s results.
The study authors noted that, for the purposes of their review, the term physiotherapy “was used for any supervised, physiotherapist-led, noninvasive treatment (mobilizations, application of ice and heat, diathermy, electrotherapy modalities).” Exercises and stretches performed by the participant at home or under physiotherapist supervision was not included in this category, and acupuncture and extracorporeal shock wave therapy were regarded as a separate intervention. Interventions with accompanying physiotherapy were grouped and analyzed separately from those with no physiotherapy, regardless of intensity and frequency.
The study authors also conducted a network meta-analysis “for treatments used by 3 or more studies for the primary outcome (pain) at late short-term (8-12 weeks) and mid-term (4-6 months) follow-up.” Primary study outcomes included pain and function, while external rotation range of motion (ER ROM) served as the secondary outcome.
“From a total of 65 eligible studies with 4,097 participants that were included in the systematic review, 34 studies with 2,402 participants were included in pairwise meta-analyses and 39 studies with 2,736 participants in network meta-analyses,” they wrote. “Despite several statistically significant results in pairwise meta-analyses, only the administration of intra-articular (IA) corticosteroid was associated with statistical and clinical superiority compared with other interventions in the short-term for pain (versus no treatment or placebo: [mean difference] MD, −1.0 visual analog scale [VAS] point; 95% CI, −1.5 to −0.5 VAS points; P< .001; versus physiotherapy: MD, −1.1 VAS points; 95% CI, −1.7 to −0.5 VAS points; P< .001) and function (versus no treatment or placebo: [standardized mean difference] SMD, 0.6; 95% CI, 0.3 to 0.9; P< .001; versus physiotherapy: SMD 0.5; 95% CI, 0.2 to 0.7; P< .001). Subgroup analyses and the network meta-analysis demonstrated that the addition of a home exercise program with simple exercises and stretches and physiotherapy (electrotherapy and/or mobilizations) to IA corticosteroid may be associated with added benefits in the mid-term (e.g., pain for IA coritocosteriod with home exercise versus no treatment or placebo: MD, −1.4 VAS points; 95% CI, −1.8 to −1.1 VAS points; P< .001).”
“In the short-term, IA corticosteroid appeared to be associated with better outcomes compared with no treatment in all outcome measures,” the study authors clarified. “Adding arthrographic distension to IA corticosteroid may be associated with positive effects that last at least as long as 12 weeks compared with IA corticosteroid alone; however, these benefits are probably not clinically significant. Compared with physiotherapy, IA corticosteroid seemed to be associated with better outcomes, with clinically significant differences. Combination therapy with IA corticosteroid plus physiotherapy may be associated with significant benefits compared with IA corticosteroid alone or physiotherapy alone for ER ROM and function, respectively, at 6 weeks. Compared with control, combined IA corticosteroid plus physiotherapy appeared to be associated with an early benefit in ER ROM (as long as 6 weeks), with clinical significance. Subacromial administration of corticosteroid appeared to be as efficacious as IA administration. The addition of acupuncture to physiotherapy did not seem to be associated with any added benefits. Based on the network meta-analysis, arthrographic distension with IA corticosteroid was probably the most effective intervention for pain at 12 weeks follow-up. IA corticosteroid alone ranked second, and as demonstrated by the pairwise meta-analysis, the benefit of adding distension appeared clinically nonsignificant.”
Millar and colleagues noted that the National Institute of Health and Care Excellence (NICE) guidelines recommend a stepped approach to treating frozen shoulder, starting out with physiotherapy and only adding IA corticosteroids if there is no, or slow, progress — however, the study authors argued that they “provide convincing evidence that IA corticosteroid is associated with better short-term outcomes than other treatments, with possible benefits extending in the mid-term; therefore, we recommend its early use with an accompanying home exercise program. This can be supplemented with physiotherapy to further increase the chances of resolution of symptoms by 6 months.”
They added that, while the majority of the patients included in this analysis had duration of symptoms of less than one year, included studies that had patients with symptoms over one year reported equally substantial improvements in outcomes, including ROM and function, suggesting that this population may also benefit from early IA corticosteroids.
Millar and colleagues acknowledged several limitations to their study—the study could not draw conclusions about effective management in specific disease stages; frequency, duration, and intensity of home exercise programs were not taken into account; and physiotherapy interventions were grouped and analyzed together regardless of nature and duration, and differences between physiotherapy methods were not assessed.
-
A systematic review of studies assessing treatment options for adhesive capsulitis, or frozen shoulder, found that early treatment with intra-articular corticosteroids consistently led to improved short-term outcomes.
-
The study authors argued that IA corticosteroids should be used early in the course of treatment alongside a home exercise program.
John McKenna, Associate Editor, BreakingMED™
The review was funded by grant MR/R020515/1 from the Medical Research Council U.K.
The study authors had no relationships to disclose.
Cat ID: 438
Topic ID: 437,438,438,737,730,192,925

