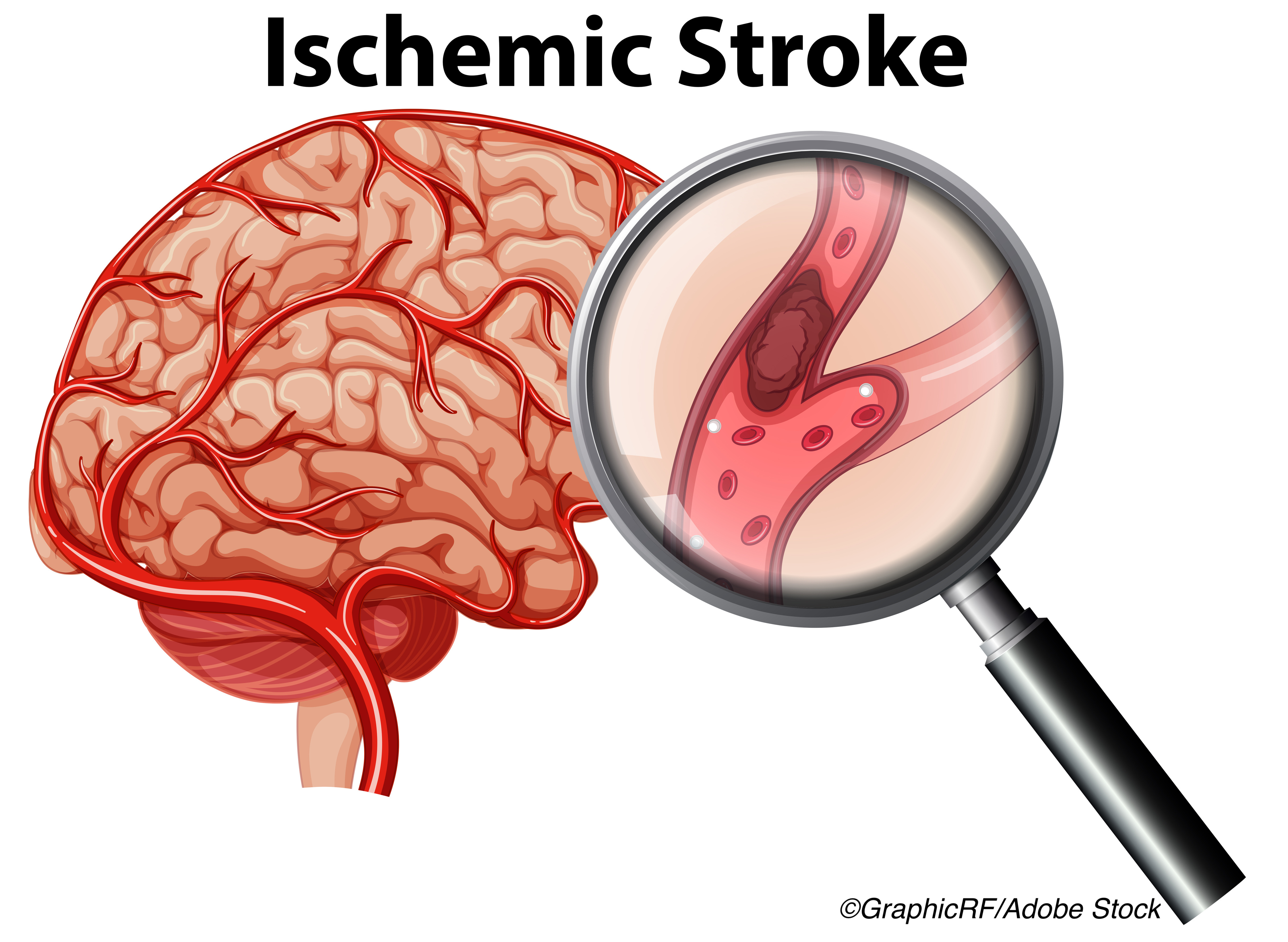
TREAT-CAD results did not establish the non-inferiority of aspirin versus vitamin K antagonists in the treatment of cervical artery dissection. Further, researchers found that patients treated with aspirin experienced more ischemic strokes, more subclinical ischemic MRI lesions, and more hemorrhagic MRI lesions.
“The evidence to consider aspirin as the standard of care in patients with cervical artery dissection is weak. Currently, it does not seem justified to replace the traditional standard treatment (anticoagulation) with aspirin, although the superiority of anticoagulation has also not been shown,” Stefan T. Engelter, MD, of the University Hospital Basel and the University Hospital for Geriatric Medicine Felix Platter, University of Basel, Basel, Switzerland, and co-authors wrote in Lancet Neurology.
For their multicenter, randomized, open-label, non-inferiority TREAT-CAD study, Engelter and colleagues enrolled 194 patients from 10 stroke centers in Switzerland, Germany, and Denmark whom they randomized to treatment with aspirin or a vitamin K antagonist (54% also received heparin or low-molecular-weight heparin). Twenty-one patients did not meet criteria for per-protocol analysis, leaving 173 patients for inclusion in the per-protocol population, including 91 treated with aspirin and 82 with a vitamin K antagonist. In all, 66% had CAD involving the carotid artery, 35% the vertebral artery, and mural hematoma was the most frequent imaging characteristic on baseline MRI (95%).
The primary endpoint of the study was a composite of clinical outcomes, including stroke, major hemorrhage, or death, and MRI outcomes including new ischemic or hemorrhagic brain lesions, at 14 days (clinical and MRI outcomes) and 90 days (clinical outcomes only) after treatment initiation, and occurred in 19% of the per-protocol patients, and in 23% of those treated with aspirin compared with 15% of those treated with the vitamin K antagonist (absolute difference: 8%; 95% CI: −4 to 21; non inferiority P=0.55).
Ischemic stroke occurred in 8% of patients treated with aspirin and in none of those treated with the vitamin K antagonist, and these occurred on either day one or day seven. One patient (1%) in the vitamin K antagonist treatment group had major extracranial hemorrhage, compared with none in the aspirin group, and subclinical MRI outcomes were seen in 13% versus 15%, respectively.
MRI outcome primary endpoints occurred in 22% of patients treated with aspirin, compared with 13% of those treated with the vitamin K antagonist, and MRI outcomes were associated with clinical symptoms in 30% of the 20 patients in the aspirin group, and none of those treated with the vitamin K antagonist.
Of note, wrote Engelter and colleagues, “With one exception, all primary endpoints (clinical outcomes or MRI outcomes) occurred in patients who had either ischemic events or MRI lesions at baseline, underlining the prognostic importance of these characteristics, as suggested by previous research. However, this trial was not powered for conclusive analyses in subgroups.”
In all, 19 adverse events occurred in patients treated with aspirin, versus 26 in those treated with the vitamin K antagonist. Seven patients experienced six serious adverse events, including migraine equivalent, dizziness, allergic reaction to MRI contrast agent, and seizure, which were all more frequent in patients treated with the vitamin K antagonist.
“Ischemic stroke, major hemorrhage, or their MRI surrogates occurred in approximately one in four patients in the aspirin group (23%), but in only one in seven patients in the vitamin K antagonist group (15%). As the upper limit of the 95% CI of the resulting 8% absolute difference in primary endpoint rates between groups (i.e., 21%) exceeded the predefined margin of 12%, non-inferiority of aspirin compared with vitamin K antagonists was not shown,” concluded Engelter et al.
Scott E. Kasner, MD, of the University of Pennsylvania, Philadelphia, wrote an accompanying editorial, laying the background in which the TREAT-CAD study was performed.
“What is the best antithrombotic therapy for cervical arterial dissection? Early anticoagulation was initially the preferred treatment for this condition, but observational studies of treatments for cervical artery dissection have produced mixed results and had inherent biases, leading to uncertainty and a need for randomized trials,” he wrote.
Results from the 2015 CADISS study, the first to compare anticoagulation with antiplatelet therapy, demonstrated lower-than-expected stroke rates in patients treated with dual antiplatelet therapy and in those treated with warfarin. CADISS researchers found an absolute difference in stroke risk of only 1%-2% between these therapies but concluded that a larger study was necessary to make any definitive conclusions.
But despite being having a similar population and design, the TREAT-CAD study demonstrated a higher stroke risk in patients treated with antiplatelets compared with CADISS.
“Perhaps the difference relates to the choice of antiplatelet therapy. The TREAT-CAD trial used aspirin only, whereas CADISS permitted alternative antiplatelet agents as well as dual antiplatelet therapy, which has been shown to reduce the risk of early stroke recurrence in people with transient ischemic attack or minor stroke,” he postulated.
Kasner concluded that even with these results from the TREAT-CAD study, “there is not enough evidence to provide a specific directive for the treatment of patients with cervical artery dissection. Clinicians should rely on the consistent findings of the large trials and use dual antiplatelet therapy for approximately 21 days for most patients presenting with acute transient ischemic attack or minor stroke.”
He added that not only are more studies needed, but they must include patients presenting with ischemic stroke instead of local symptoms.
Study limitations include the large non-inferiority margin used, the large 95% CI for the primary endpoint, the use of a composite primary outcome, and the higher number of acute recanalization procedures patients treated with aspirin underwent.
Engelter and colleagues also noted: “A major limitation of the non-inferiority design is that this trial could not show that aspirin is worse than or inferior to vitamin K antagonists in the treatment of cervical artery dissection, as the study was not designed or powered to address the question of superiority of either treatment. It is important to emphasize that although aspirin was not shown to be non-inferior to vitamin K antagonists, these results do not mean that aspirin is worse than anticoagulants or that vitamin K antagonists are superior to aspirin. Moreover, as most study participants presented with minor-to-moderate strokes, transient ischemic attacks, or non-ischemic symptoms, the applicability of our key findings to patients with major or disabling stroke is not clear.”
-
In the multicenter, randomized controlled TREAT-CAD trial, researchers compared aspirin with vitamin K antagonists in the treatment of cervical artery dissection and could not establish the non-inferiority of aspirin.
-
Ischemic stroke, major hemorrhage, or their MRI surrogates occurred in approximately one in four patients in the aspirin group, but in only one in seven patients in the vitamin K antagonist group.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
The TREAT-CAD study was funded by the Swiss National Science Foundation, Swiss Heart Foundation, Stroke Funds Basel, University Hospital Basel, University of Basel, Academic Society Basel.
Engelter reported receiving grants from Swiss National Science Foundation, Swiss Heart Foundation, Freiwillige Akademische Gesellschaft Basel, University of Basel, and University Hospital Basel, during the conduct of the study.
Kasner has received grants and personal fees from Medtronic and Bristol-Myers Squibb; personal fees from AstraZeneca, Abbvie, Abbott, and UpToDate; and grants from Genentech, outside of the submitted work.
Cat ID: 130
Topic ID: 82,130,730,130,38,192,925


