Cervical cancer screening tests were significantly overused in women at average risk for cervical cancer in the United States between 2013 and 2014 despite evidence-based guidelines that caution against excess testing, a large cohort study has shown.
Almost two-thirds of approximately 2.3 million women between 20 and 65 years of age underwent repeat cervical cancer screening within 36 months of their index test, Jason Wright, MD, Columbia University College of Physicians and Surgeons New York City, and colleagues reported in JAMA Network Open. The cumulative incidence of repeat cervical cancer screening was 17.7% (95% CI, 17.6-17.7%) at one year, 51.1% (95% CI, 51.0-51.2%) at two years, and 65.8% (95% CI, 65.7-65.8%) at three years, they added.
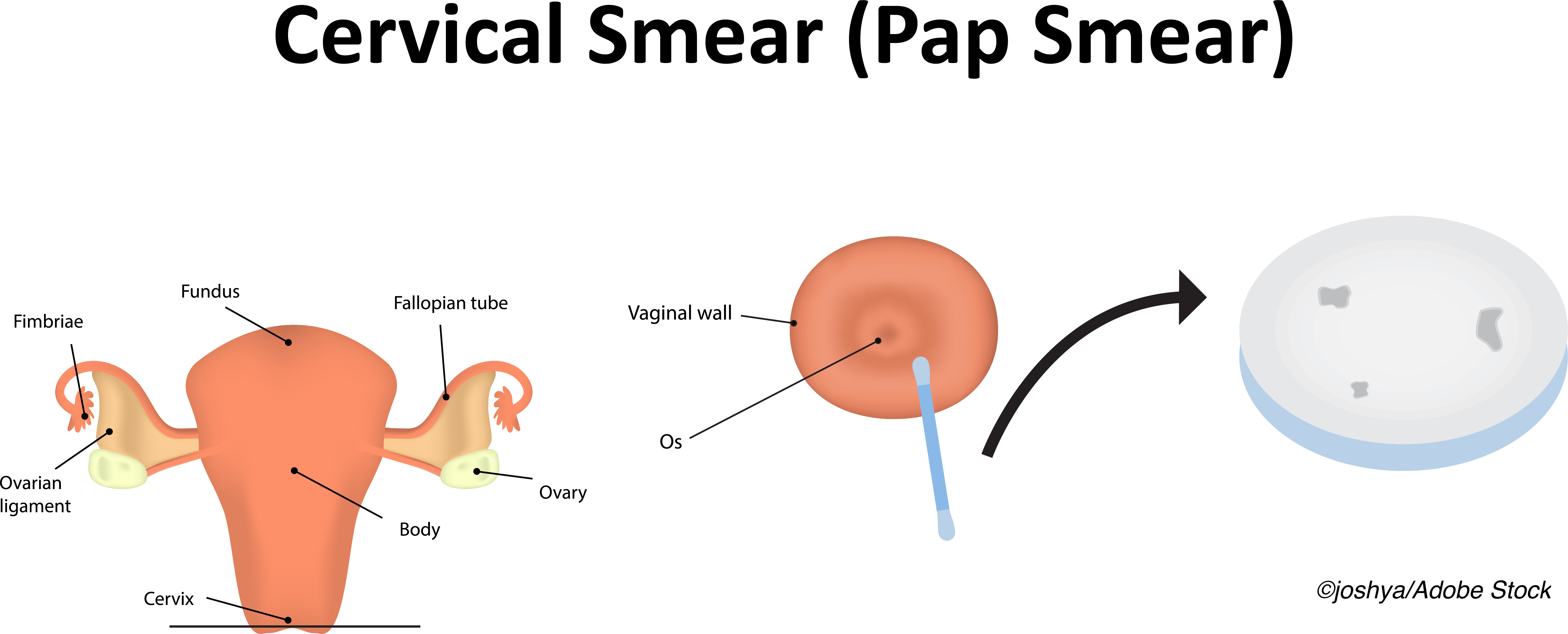
“The 2012 American Cancer Society guidelines for cervical cancer screening recommend use of cytologic screening every three years or co-testing with HPV and cytological testing every five years in women aged 30 to 65 years,” Wright and colleagues observed. “…The findings of this cohort study suggest that among commercially insured women with average risk who underwent cervical cancer screening in 2013 to 2014, cervical cancer screening tests were frequently overused.”
A total of 2,299,177 women, median age of 47 years (interquaritle range [IQR], 39-54 years), were identified in the MarketScan database. Women had underdone cervical cancer screening with either cytologic testing, co-testing or primary HPV testing in 2013 through to 2014 and were followed up for three years. Some 55.9% of women underwent cytologic testing alone, 43.1% underwent co-testing, and only 0.9% underwent primary HPV testing during the study interval.
Compared with women who were initially screened with co-testing, repeat testing was 86% more common among women initially screened with cytology at an adjusted Odds Ratio (OR) of 1.86 (95% CI, 1.85-1.88), the investigators noted. However, it was 37% less likely in women who were screened with primary HPV testing at an OR of 0.63 (95% CI, 0.61-0.66).
Among their other findings:
- Patients who were diagnosed with a sexually transmitted infection after their index screening test were also 42% more likely to undergo repeat testing at an OR of 1.42 (95% CI, 1.21-1.68).
- Repeat screening was less common in women between the ages of 60 to 64 compared to women 30 to 39 years of age (P<0.001).
- Women with two or more comorbidities were also less likely to undergo repeat screening than those with no comorbidities (P<0.001) as were women screened with co-testing compared with women who underwent cytologic testing alone (P<0.001).
- Women who were pregnant, who had gynecologic symptoms and those with mental health or substance abuse issues were similarly less likely to undergo repeat screening.
- Almost 47% of women in the overall cohort underwent a repeat screening test in year two after their index test and in this group of women, over one-third at 35.3% had a repeat screening test 12 to 24 months after their index screen, while 47.2% of those who did not have a screening test two to 12 months after their initial screening test underwent repeat testing within 12 to 24 months.
- The median time between the screening test at 2 years and the prior screening evaluation was 13.4 months.
- Almost 45% of women underwent a repeat screening test 24 to 36 months after their initial index test.
- The median time between the cervical cancer screening test at year three and the prior test was 14.5 months (IQR, 12.6-26 months).
- During the second year, almost all women at 96.7% of the cohort who had undergone interval screening had had a gynecological examination compared with only 26.2% of women who had not had cervical cancer screening in that year (P<0.001).
- A virtually identical percentage of women who had undergone cervical cancer screening during year three also underwent a gynecological examination compared with only about 23% of women who did not undergo cervical cancer screening in year three.
“Overtesting was particularly common in younger women and in women screened with cytologic testing alone,” the authors wrote. “[And as] current guidelines recommend screening no more often than every five years in women who have undergone HPV testing, our findings would likely have been even more pronounced if follow-up were extended beyond 36 months.”
As Wright and colleagues observed, overuse of cervical cancer screening has significant consequences, among them the fact that low-grade abnormal findings are likely to result in further diagnostic testing including colposcopy and biopsy and even ablative or excisional procedures.
“These procedures are often associated with psychological stress and physical symptoms,” they wrote. “Furthermore, treatment of preinvasive cervical lesions is associated with adverse pregnancy outcomes, including preterm birth.”
They did note that factors that might influence overuse of cervical cancer screening include frequent changes and differences in multiple societal guidelines. Women may also forget when they last underwent cervical cancer screening, which could result in too frequent screening, the investigators suggested.
“Even if women are aware of screening guidelines and their [own] history, they often prefer to continue annual cervical cancer screening,” Wright and colleagues wrote.
Similarly, physicians often fear that less frequent screening will lead to disengagement from gynecologic services, and they may also be concerned about medical liability if they do extend the interval between screenings to better align with current guidelines.
“There is currently minimal financial disincentive for clinicians to perform more frequent testing,” the authors wrote and added, “Evaluation of interventions to align clinical practice with evidence-based guidelines for cervical cancer screening [is] clearly needed to help reduce patient harm and medical waste.”
-
Cervical cancer screening tests were significantly overused in women at average risk for cervical cancer in the United States between 2013 and 2014 despite evidence-based guidelines that caution against excess testing, a large cohort study has shown.
-
Identification of low-grade abnormalities during the unnecessary cervical cancer screening can lead to further diagnostic testing and adverse psychological and physical consequences for patients.
Pam Harrison, Contributing Writer, BreakingMED™
Research was supported by the Herbert Irving Comprehensive Cancer Center.
Wright reported receiving grants from Merck as well as personal fees from Clovis Oncology and UpToDate.
Cat ID: 692
Topic ID: 78,692,730,692,693,192,925


