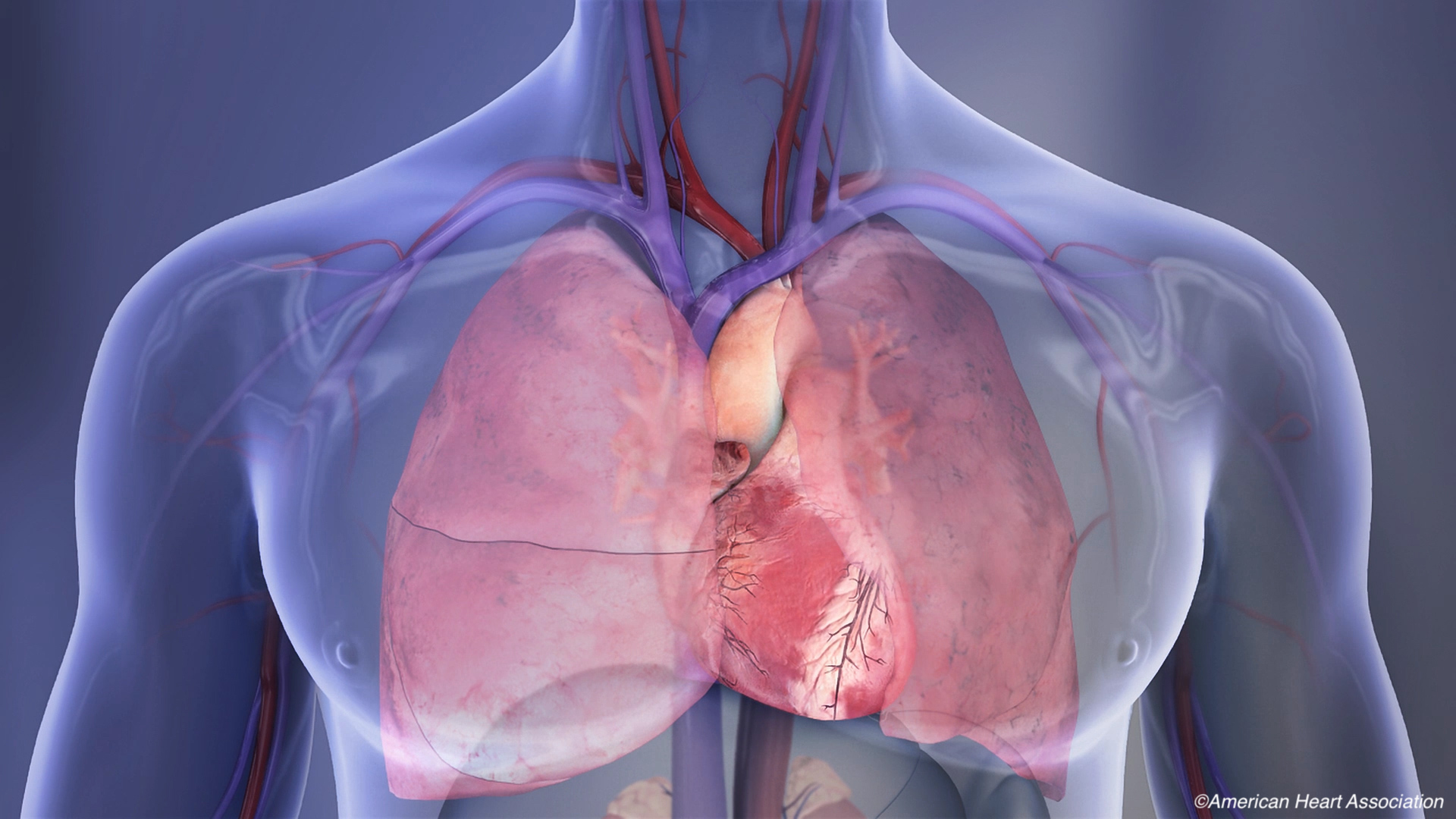
The American Heart Association and the American College of Cardiology have jointly issued a new guideline focused solely on chest pain. Entitled “2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/ SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines,” the guidelines were published simultaneously in Circulation and the Journal of the American College of Cardiology.
The goal of the new guidelines, the first to focus solely on the evaluation and diagnosis of chest pain, is to help clinicians and other medical professionals use standardized risk assessments, clinical pathways, and tools to aid in diagnosis of individuals experiencing chest pain. Recommendations are based on a comprehensive literature search conducted from November 11, 2017, to May 1, 2020.
“Everyone should know the symptoms that can indicate a heart attack and that calling 911 is the most important thing to do to save their life or that of their loved one experiencing chest pain,” said Martha Gulati, MD, MS, Chair of the guideline writing group and professor of cardiology and former academic division chief of the division of cardiology at the University of Arizona in Phoenix. “This standard approach provides clinicians with the guidance to better evaluate patients with chest pain, identify patients who may be having a cardiac emergency and then select the right test or treatment for the right patient.”
Roughly 5% of adults presenting to the ED with chest pain will have acute coronary syndrome (ACS), and over 50% will be diagnosed with a non-cardiac cause for the pain. Thus, according to the AHA/ACC, an assessment of the severity and cause of the chest pain is imperative. Clinicians are advised to use standard risk assessments to determine whether that patient is at low, intermediate, or high risk for a cardiac event.
For healthcare professionals in the emergency department, the initial goals of evaluating adults presenting with chest pain are to identify any life-threatening causes of the pain, and determine the need for hospitalization or testing. In this setting, thorough screening is recommended to assess the patient’s risk—high, intermediate, or low—for a cardiac event.
Patients at low risk should be referred for additional outpatient evaluation.
“When some people arrive in the emergency department with chest pain, they often won’t need additional or immediate testing, and the health care team should explain to the patient and their family the various initial tests and risk assessment and their risk level,” said Gulati in a press release. “Often, patients have additional concerns because they fear a heart attack or other severe cardiac event, which is understandable. However, we have advanced tools that help us determine whether a cardiac emergency or severe heart event is likely or not.”
In defining chest pain, the guidelines recommend the following: “Chest pain should not be described as atypical, because it is not helpful in determining the cause and can be misinterpreted as benign in nature. Instead, chest pain should be described as cardiac, possibly cardiac, or noncardiac because these terms are more specific to the potential underlying diagnosis.”
This strong Class 1 recommendation is based on moderate quality evidence from one or more well-designed, well-executed nonrandomized trials, observational studies, registry studies, or a meta-analysis of these.
Chest radiography is recommended in patients presenting with acute chest pain to “evaluate for other potential cardiac, pulmonary, and thoracic causes of symptoms.” Biomarker testing including serial cardiac-specific troponin (1 or T) levels are recommended to identify abnormalities and patterns that indicate acute myocardial injury. The guidelines specifically cite high-sensitivity cTn as the preferred biomarker, due to its rapidity and ability to increase accuracy of diagnosis.
Of note, the guidelines specify that there is no benefit to the use of creatine kinase myocardial (CK-MB) isoenzyme and myoglobin, in lieu of cTn testing.
“While there is no one ’best test’ for every patient, the guideline emphasizes the tests that may be most appropriate, depending on the individual situation, and which ones won’t provide additional information; therefore, these tests should not be done just for the sake of doing them,” added Gulati.
“Appropriate testing is also dependent upon the technology and screening devices that are available at the hospital or health care center where the patient is receiving care. All imaging modalities highlighted in the guideline have an important role in the assessment of chest pain to help determine the underlying cause, with the goal of preventing a serious cardiac event,” she concluded.
The guidelines specify that women are unique when presenting with symptoms of ACS, and while chest pain is the most common symptom experienced by both men and women, women are more likely to have concomitant symptoms, including nausea and shortness of breath.
Two Class 1 recommendations are directed specifically at women. The first states that “Women who present with chest pain are at risk for underdiagnosis, and potential cardiac causes should always be considered.” The second recommends obtaining “a history that emphasizes accompanying symptoms that are more common in women with ACS.”
The guidelines also stressed the importance of shared decision-making and the regular use of clinical decision pathways both in the emergency department and outpatient settings.
The AHA/ACC summed up its guideline recommendation with two acronyms:
- Chest pain means more than pain in the chest.
- High-sensitivity troponins preferred.
- Early care for acute symptoms.
- Share the decision-making.
- Testing not routinely needed in low-risk patients.
- Pathways: Use clinical decision pathways.
- Accompanying: Women may be more likely to present with accompanying symptoms.
- Identify patients most likely to benefit from further testing.
- Noncardiac is in. Atypical is out.
- Structured risk assessment should be used.
-
The goal of the new guidelines, the first to focus solely on the evaluation and diagnosis of chest pain, is to help clinicians and other medical professionals use standardized risk assessments, clinical pathways, and tools to aid in diagnosis of individuals experiencing chest pain.
-
Be aware that roughly 5% of adults presenting to the ED with chest pain will have acute coronary syndrome (ACS), and over 50% will be diagnosed with a non-cardiac cause for the pain.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
Gulani reported no disclosures.
Cat ID: 254
Topic ID: 253,254,254,730,914,192,925

