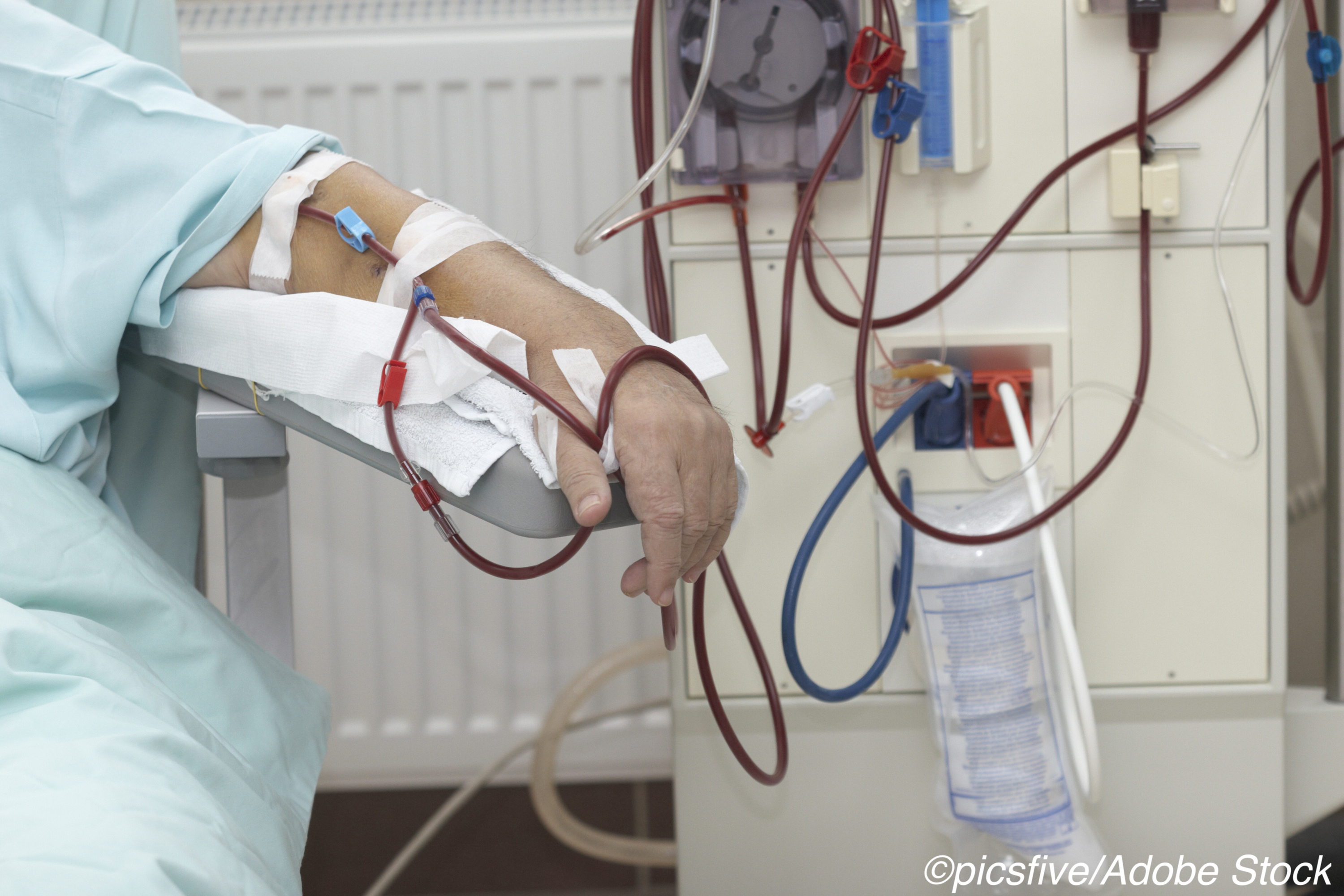
The Centers for Medicare & Medicaid Services (CMS) suggested changes to the Medicare End-Stage Renal Disease (ESRD) Prospective Payment System (PPS) in an effort to support and expand access to at-home dialysis.
“CMS is proposing to expand the transitional add-on payment adjustment for new and innovative equipment and supplies (TPNIES) that was introduced last year to now cover qualifying new dialysis machines when used in the home,” CMS explained in a press release. “This would provide a new payment mechanism to expand access to certain new and innovative home dialysis machines, facilitating quicker availability to Medicare beneficiaries.”
In their announcement, CMS pointed out that more than 85% of Medicare beneficiaries with ESRD currently receive dialysis in a qualified facility a minimum of 3 times a week. However, the agency noted that this population also has the highest rate of Covid-19 hospitalizations among Medicare recipients, “highlighting the importance that this population stay at home during the public health emergency to reduce risk of exposure to the virus.
“In order to ensure that dialysis patients have access to the best possible care, CMS is proposing needed innovative changes to encourage more home dialysis treatment,” the agency wrote.
This new proposal, according to CMS, would build on previous actions intended to improve care in Medicare patients with kidney disease, including:
- “The proposed ESRD Treatment Choices (ETC) Model that would encourage greater use of home dialysis and kidney transplants for Medicare beneficiaries with ESRD in order to preserve or enhance their quality of care while reducing Medicare expenditures.
- “The Kidney Care First (KCF) and Comprehensive Kidney Care Contracting (CKCC) Options of the Kidney Care Choices (KCC) Model that will test whether new care delivery and Medicare payment options can improve the quality of care and reduce the total cost of care for patients with kidney disease.
- “Refinements to eligibility for the transitional drug add-on payment adjustment (TDAPA) under the ESRD PPS to better target the additional payment to innovative renal dialysis drugs and biological products based on the Food and Drug Administration’s (FDA’s) New Drug Application Classifications.”
For a fact sheet outlining the proposed rule, click here. To view the proposed rule on the Federal Register website, click here.
John McKenna, Associate Editor, BreakingMED™
Cat ID: 127
Topic ID: 81,127,730,127,192,463

