Among patients with relapsing-remitting multiple sclerosis (MS), treatment with the B-cell targeting leukemia drug ofatumumab was associated with lower relapse rates than treatment with the FDA approved MS drug teriflunomide in phase III findings from the ASCLEPIOS I and II trials.
Treatment with both drugs was associated with low overall annualized relapse rates in the two simultaneously conducted, active-controlled trials, funded by ofatumumab-marketer Novartis.
But the relapse rate was significantly lower in the ofatumumab-treated patients in both trials (0.11 vs 0.22, respectively, in trial 1 [difference, −0.11; 95% CI, −0.16 to −0.06; P<0.001] and 0.10 versus 0.25 in trial 2 [difference, −0.15, 95% CI, −0.02 to −0.09; P<0.001]).
The two treatment groups did not show significant differences in confirmed improvement in MS-related disability.
Findings from the ASCLEPIOS I and ASCLEPIOS II trials were presented as a platform presentation at the CMSC virtual meeting and published online August 5 in The New England Journal of Medicine.
A post hoc analysis of the two trials, reported in late May, showed ofatumumab to be associated with a significantly higher rate of achieving no evidence of disease activity (NEDA-3) compared to teriflunomide in the first year of treatment (47.0% vs 24.5%; P<0.001) and the second year (87.8% vs 48.2%; P<0.001).
In early June, Novartis announced that, despite the positive trial findings, the FDA was extending its review of the company’s Supplemental Biologics License Application (sBLA) for ofatumumab as an MS therapy until September.
Ofatumumab, marketed as Arzerra for chronic lymphocytic leukemia, is an anti-CD20 monoclonal antibody given once a month by self-administered injection.
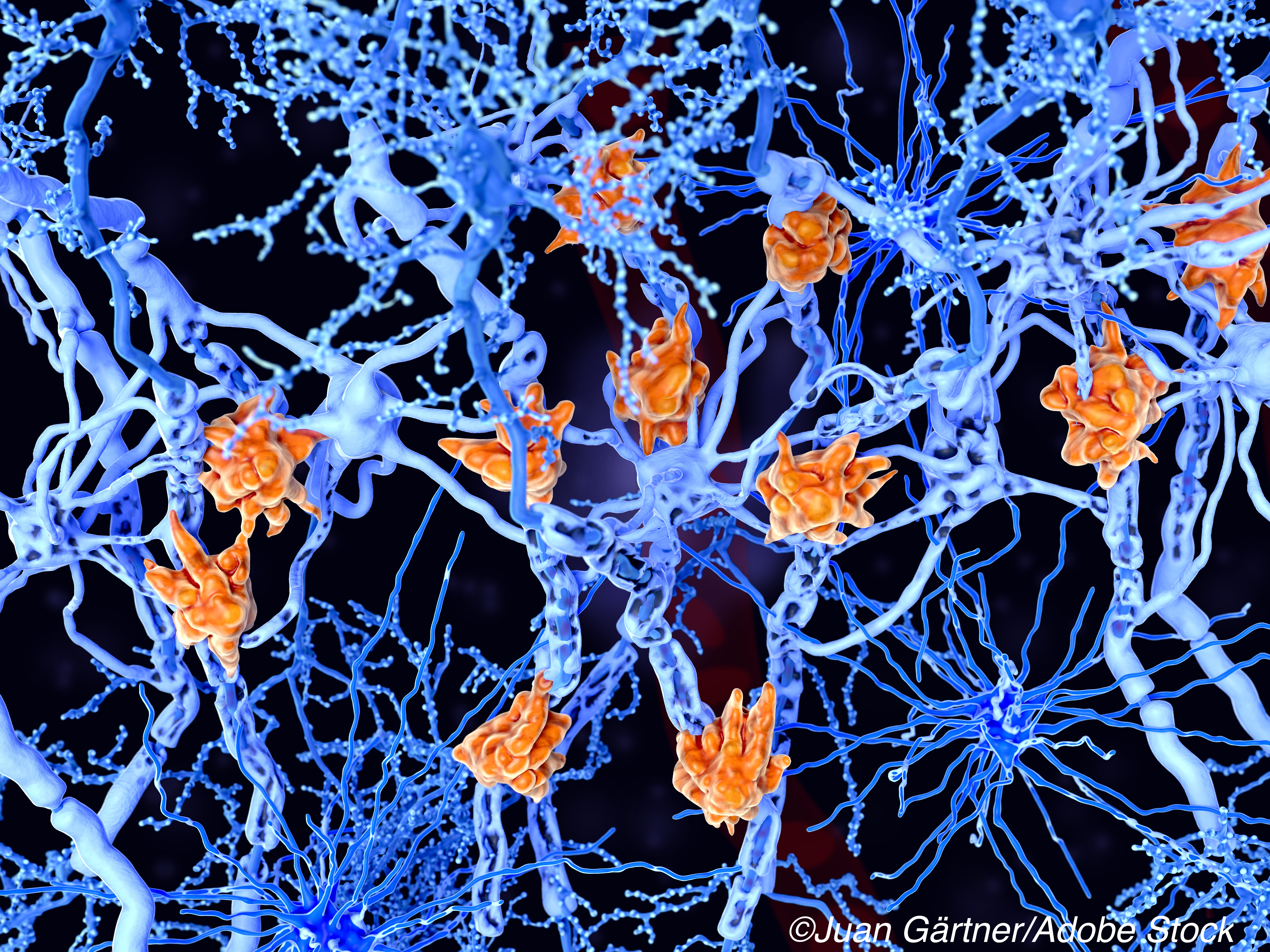
“The pathophysiology of multiple sclerosis involves B cells,” wrote ASCLEPIOS trial researchers Stephen L. Hauser, MD, of the University of California, San Francisco, and colleagues in NEJM. “Anti-CD20 monoclonal antibodies that induce B-cell depletion, such as rituximab and ocrelizumab, are effective disease modifying therapies for multiple sclerosis.”
Ofatumumab binds to a region distinct from that of other anti-CD20 antibodies, including the smaller and the larger loop of CD20 receptors.
In the two double-blind, double dummy phase III ASCLEPIOS trials, patients with relapsing-remitting MS were randomly assigned to treatment with subcutaneous ofatumumab (20 mg every 4 weeks after 20-mg loading doses at days 1, 7, and 14) or oral teriflunomide (14 mg daily) for up to 30 months.
The study’s primary endpoint was the annualized relapse rate, and secondary endpoints included disability worsening confirmed at 3 months or 6 months, disability improvement confirmed at 6 months, the number of gadolinium- enhancing lesions per T1-weighted magnetic resonance imaging (MRI) scan, the annualized rate of new or enlarging lesions on T2-weighted MRI, serum neurofilament light chain levels at month 3, and change in brain volume.
From Oct. 2016 through March 2018, a total of 1,882 patients were enrolled in the trials at 385 sites in 37 countries, including 946 randomized to the ofatumumab arm of the studies and 936 randomized to the teriflunomide arm. The median follow-up was 1.6 years.
In addition to the annualized relapse rate findings, the study revealed:
- A lower percentage of patients with disability worsening confirmed at 3 and 6 months in the ofatumumab group, but no significant difference in the two groups in confirmed disability improvement.
- In the pooled trials, the percentage of patients with disability worsening confirmed at 3 months was 10.9% with ofatumumab and 15.0% with teriflunomide (hazard ratio, 0.66; P=0.002); the percentage with disability worsening confirmed at 6 months was 8.1% and 12.0%, respectively (hazard ratio, 0.68; P=0.01); and the percentage with disability improvement confirmed at 6 months was 11.0% and 8.1%, respectively (hazard ratio, 1.35; P=0.09).
- Ofatumumab was superior to teriflunomide in suppressing lesion activity on MRI.
- Injection-related reactions occurred in 20.2% in the ofatumumab group and in 15.0% of the teriflunomide group, and serious infections occurred in 2.5% and 1.8% of the patients, respectively, in the two groups.
“Ofatumumab was associated with lower annualized relapse rates than teriflunomide and showed benefit with respect to most secondary clinical and MRI endpoints, but not confirmed disability improvement,” Hauser and colleagues wrote.
They concluded that the trials do not “permit any inferences to be made about the efficacy of ofatumumab as compared with other drugs for multiple sclerosis that are considered to be more potent than teriflunomide.”
“Larger and longer trials are required to determine the long-term effect and risks of ofatumumab as compared with other disease-modifying treatments, including other anti-CD20-monoclonal antibodies,” they added.
-
In combined phase III findings from the ASCLEPIOS I and II trials, treatment with the B-cell targeting leukemia drug ofatumumab was associated with lower relapse rates than treatment with the MS drug teriflunomide in patients with relapsing-remitting multiple sclerosis.
-
Be aware that this activity describes an off-label use of a drug.
Salynn Boyles, Contributing Writer, BreakingMED™
Both studies were supported by Novartis Pharma.
Hauser served as a member of scientific advisory boards or consultant for Alector, Annexon Biosciences, Bionure, Molecular Stethoscope, Nerona Therapeutics, and Symbiotix. He received stock options from Alector, Annexon Biosciences, Bionure, Molecular Stethoscope, Neurona Therapeutics, and Symbiotix. He received travel grants from F. Hoffmann-LaRoche AG and Novartis.
Cat ID: 130
Topic ID: 82,130,730,130,36,764,192,763


