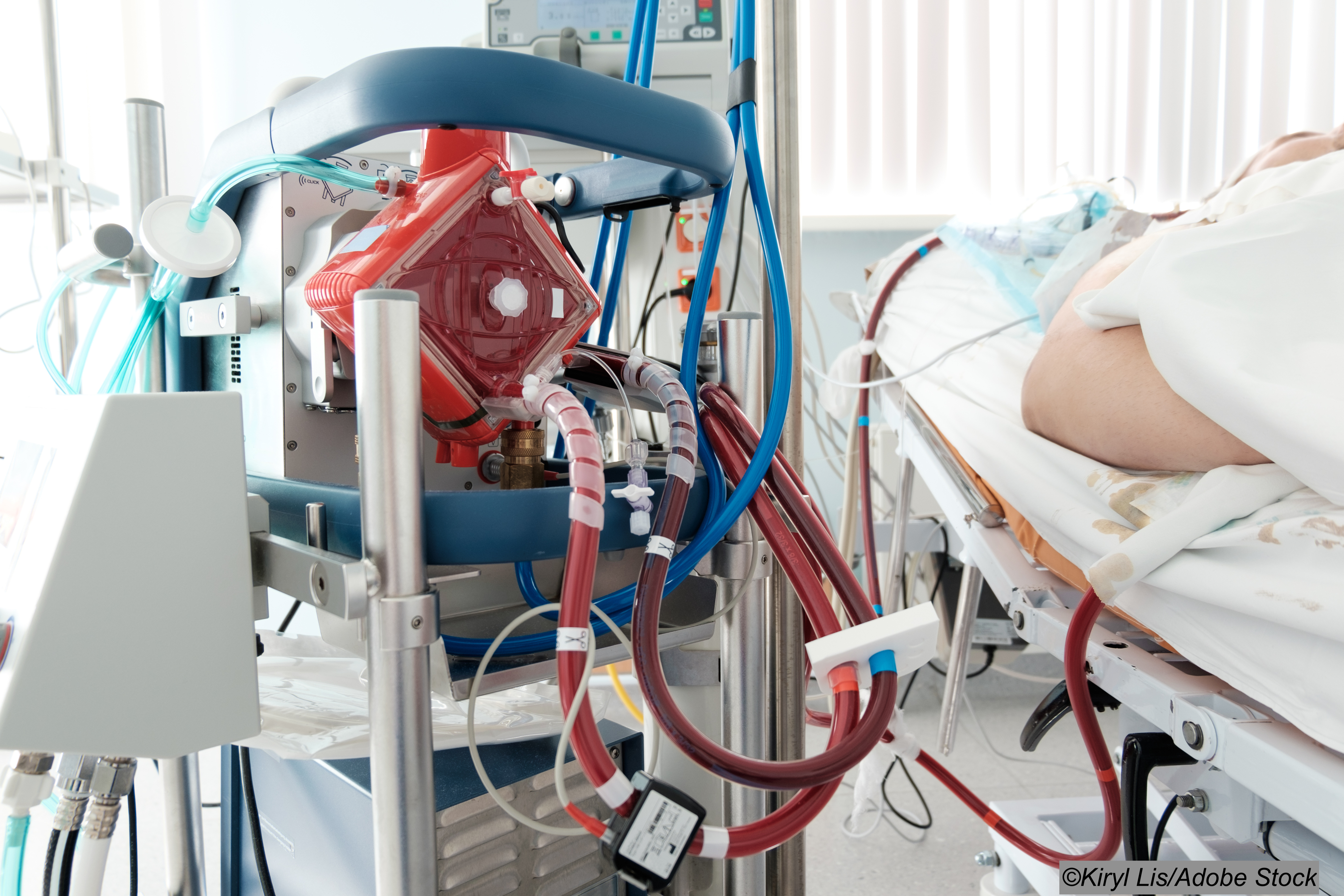
The death rate among critically ill Covid-19 patients on extracorporeal membrane oxygenation (ECMO) significantly increased in the latter months of 2020, compared to earlier on in the pandemic, according to registry data involving 4,812 patients treated in 41 countries.
The analysis of outcomes among Covid-19 patients on ECMO showed, as other studies have, a substantial survival benefit for patients treated at institutions with experience delivering ECMO prior to the pandemic, compared to late-adopting centers with less experience.
Ninety-day in-hospital mortality following ECMO support among Covid-19 patients in 2020 increased by roughly 15% after May of 2020, compared to mortality before May 2020. The median duration of ECMO support also increased by 6 days.
Patients supported with ECMO after May 1 were more likely to receive corticosteroids, and they also had a higher incidence of treatment-refractory disease, despite having similar risk factors to patients treated before this date.
The ELSO registry finding of worsening ECMO mortality over the course of the Covid-19 pandemic, published online in The Lancet, highlights the need for “continued surveillance, facilitating awareness of local and regional mortality rates, duration of ECMO support, and resource constraints,” wrote researcher Ryan Barbaro, MD, of the University of Michigan, Ann Arbor, and colleagues.
“Our findings have important implications, both in setting expectations with patients and surrogate decision makers, and for informing clinicians and policy makers with respect to the most appropriate ECMO initiation criteria,” they wrote. “Furthermore, centers should consider developing local policies that guide the ethical allocation of ECMO when resources are constrained.”
For the purposes of the study, early-adopting center were defined as those using ECMO support for Covid-19 from the start of the pandemic. Late-adopting centers were defined as those providing ECMO for Covid-19 beginning after May 1, 2020. The primary study outcome was in-hospital mortality within 90 days of ECMO initiation, and Cox proportional hazards modeling was used to compare patient and center-level adjusted relative risk of mortality among three groups.
Those groups included Covid-19 patients placed on ECMO May 1 or earlier (group A1), patients starting ECMO between May 2 and Dec. 31, 2020 (group A2), and ECMO patients managed at late-adopting centers offering the life support option after May 1, 2020.
The analysis of data from the 349 centers worldwide revealed:
- Among early adopting centers, in-hospital mortality 90 days after ECMO initiation was 36.9% (95% CI 34.1-39.7) among patients who started ECMO on or before May 1 versus 51.9% (95% CI, 50.0-53.8) among those placed on ECMO after May 1.
- Among late-adopting centers (group B), 90-day mortality was 58.9% (95% CI, 55.4-62.3).
- Relative to patients placed on ECMO later in the pandemic, those placed on ECMO before May 1 had a lower adjusted relative risk of in-hospital mortality 90 days after ECMO (hazard ratio 0.82; 95% CI, 0.70-0.96).
- Patients treated at later-adopting centers had a higher adjusted relative risk for death within 90 days (ARR, 1.42; 95% CI, 1.17-1.73).
Of note: “Advanced age, cancer, cardiac arrest before starting ECMO, and acute kidney injury were associated with an increased relative risk of mortality,” the study authors wrote.
A study limitation cited by the researchers was the voluntary nature of participation and data entry into the ELSO Registry, and the lack of external validation of cases submitted to the registry.
In an accompanying commentary, critical care physician Alain Vuylsteke of Royal Papworth Hospital, Cambridge, U.K., wrote that the rationalization for ECMO is that it is less damaging to the lungs than traditional invasive mechanical ventilation because it decreases physiological insult.
“This hypothesis is elegant but ECMO has never been proven to be superior to not using ECMO in randomized controlled trials,” Vuylsteke wrote.
“Barbaro and colleagues show that, later in the pandemic, patients more often had non-invasive ventilation before ECMO and were given steroids or other specific Covid-19 therapies. The latter is probably reflected in the post-May 1 cohorts. Clinicians rely on an experience they do not yet have to allocate patients to ECMO and might miss important characteristics. It is not surprising that outcomes are changing as the pandemic is processing.”
Vuylsteke noted that it is not clear if “some patients survived despite ECMO they did not need, or if some died just because of ECMO, or what happened to those who were denied ECMO.”
“This is the conundrum to clarify before we decide if ECMO is worth using or not,” he wrote.
“ECMO cannot be blamed for the increased mortality; it is merely a tool and clinicians still need to understand when to use it for the greatest benefit… To date, thousands of patients with Covid-19 have been ventilated in intensive care and a proportion had access to ECMO. Collating and analyzing their clinical journeys might help to clarify if ECMO is a tool to keep,” he added.
-
The death rate among critically ill Covid-19 patients on extracorporeal membrane oxygenation (ECMO) significantly increased at early-adopting centers in the latter months of 2020, compared to the early months of the pandemic.
-
Patients experienced a substantial survival benefit when treated at institutions with experience delivering ECMO prior to the pandemic, compared to late-adopting centers with less experience.
Salynn Boyles, Contributing Writer, BreakingMED™
The researchers reported no source of funding support. Lead researcher Ryan Barbaro is the ELSO Registry chair, and other researchers reported being on the registry’s board of directors or serving as executives for the registry. Researcher Daniel Brodie is chair of the execuutive committee for the International ECMO Network.
Cat ID: 190
Topic ID: 79,190,730,933,190,926,151,928,195,929,925,934