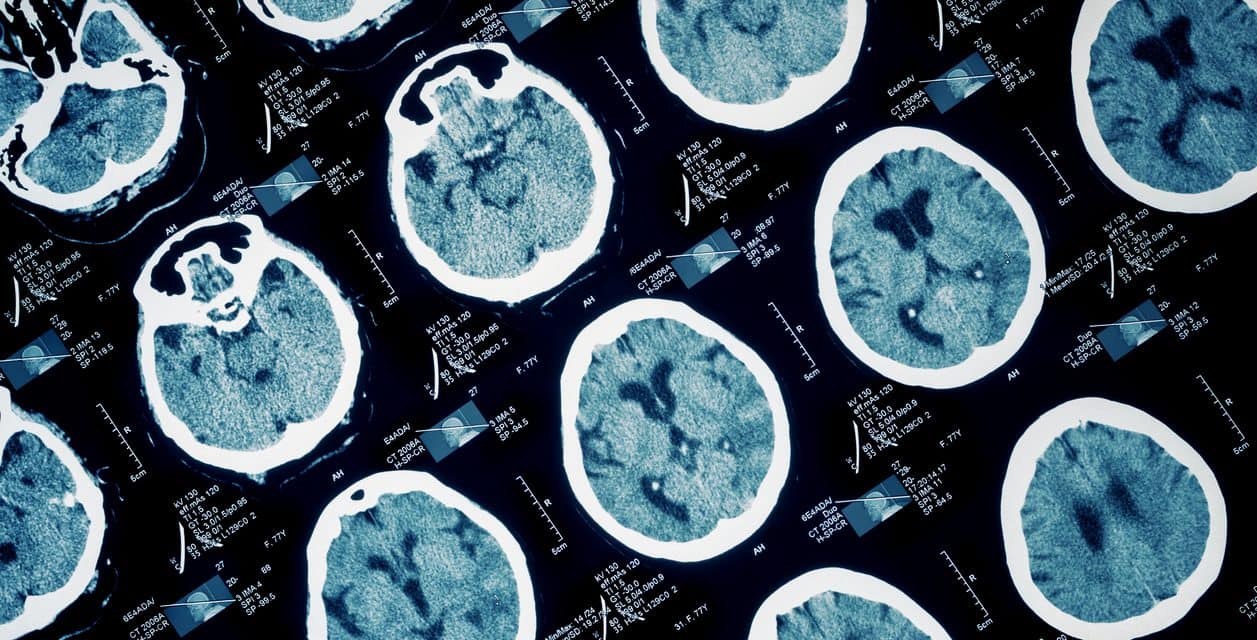
About 1% to 3% of the United States population has treatment-resistant depression (TRD), a costly and disabling disorder. In recent clinical trials, deep brain stimulation (DBS) has been used on various neuroanatomic targets in the brain in an effort to treat TRD. Helen S. Mayberg, MD, and colleagues in Toronto published a report in 2005 which demonstrated encouraging results when using DBS in the subcallosal cingulate (SCC) matter, an area of the brain that has been dubbed “Area 25.” In this study, patients with TRD who had DBS experienced antidepressant response rates in excess of 50% when assessed 6 and 12 months after the procedure. “Although results were encouraging, this initial pilot study was limited by being an open-label investigation,” says Dr. Mayberg.
In an effort to garner more long-term efficacy and safety data on SCC DBS for TRD and extend experience with the procedure, Dr. Mayberg teamed up with Paul E. Holtzheimer, MD, and colleagues at Emory University and published a study in the February 2012 Archives of General Psychiatry involving 17 TRD patients who received the procedure. The analysis also aimed to address whether there was an antidepressant effect associated with sham SCC DBS and if the procedure was safe and effective in patients with treatment-resistant bipolar depression. (see also, Navigating Patients Through Depression)
Analyzing the New Data on DBS
In the study by Drs. Holtzheimer and Mayberg, participants received single-blind sham SCC DBS for 4 weeks, in which patients did not know if the DBS system was on or off. This was followed by active stimulation for 24 weeks. Patients were evaluated for up to 2 years after the onset of active stimulation. No psychotropic medications were added and no dosages were increased for any patient during the 4 weeks prior to surgery until entry into the observational phase after 24 weeks of active stimulation.
“Overall, chronic DBS was safe and well tolerated, and no hypomanic or manic episodes occurred.”
Patients in the study experienced significantly less depression and higher function when continuing SCC DBS. “After 2 years of active stimulation, 58% of patients achieved remission, meaning they were essentially well, and 92% responded to SCC DBS, meaning their symptoms improved by at least 50%,” says Dr. Holtzheimer (Table). “Remission and response were seen in 18% and 41% of patients after 24 weeks and in 36% and 36% of patients after 1 year of active stimulation.” (see also, A Tool to Assess Depression Remission)
Cutoffs of average scores on the Hamilton Depression Rating Scale were used to group patients into remission, mild depression, or moderate-to-severe depression at each time point (Figure). “No patient achieving remission at 2 years experienced a spontaneous relapse,” Dr. Holtzheimer says. “Efficacy was also similar for patients with major depressive disorder and those with bipolar II disorder. Overall, chronic DBS was safe and well tolerated, and no hypomanic or manic episodes occurred.”
More Studies on Remission with DBS the Way
Although results were encouraging, the findings should be interpreted with caution. “The clinical improvements could be explained by a sham stimulation effect that persisted beyond the 4-week sham lead-in,” says Dr. Holtzheimer. “A longer, randomized, sham-controlled trial is needed to adequately test this. However, our overall findings argue against a clinically significant sham DBS effect.”
Nearly all patients experienced some improvement in depression severity, with most achieving remission after 2 years of SCC DBS. However, it took longer for some patients to improve during the course of the study. “The reasons for this are unclear and warrant further study,” says Dr. Mayberg. “Furthermore, our data needs to be replicated in larger trials. A better understanding of how DBS works for TRD will hopefully emerge. More safety data from future trials is also required.” (see also, DBS for Treatment-Resistant Depression)
A Bright Future for Patients with Treatment-Resistant Depression
DBS is not yet approved by the FDA for use in TRD so it can only be offered in clinical trial settings for now. The potential for this treatment approach, however, is enormous, says Dr. Holtzheimer. “The currently available therapies for TRD are limited, and these patients have often been in a depressed state for years. Many are disabled and isolated.” Dr. Mayberg adds that as DBS is further developed and refined for use in TRD, there is hope that a greater number of patients will benefit from it. “Additional studies will be needed to identify which patients are appropriate candidates and when DBS should be considered in the course of illness. SCC is not the only brain area being tested. Identifying which target is best for a given patient is a next step once the different targets now being studied are proven safe and effective in large scale clinical trials. There is still more that we need to discover, but we’re optimistic that DBS has potential to treat TRD based on our early findings.”