Welcome to a new blog by Philomena Asante, MD, MPH, that will highlight a healthcare institution, medical educational program, or professional medical organization striving to promote diversity, equity, inclusion, and justice in medicine. We know racism and bias exist in medicine. Now, it’s time to focus on solutions.
In this post, Dr. Asante interviews Jordan Spector, MD, the Emergency Medicine Residency Program Director at Boston Medical Center. Dr. Spector discusses the importance of diversity in medicine and describes strategies used in his residency program to recruit a diverse group of resident physicians.
PA: Tell me why diversity in medicine is important to you and how it plays into your role as a residency program director.
JS: I’m still learning in many of these domains and acknowledge I come from a place of privilege. I certainly didn’t grow up rich, but I have not had to suffer in life, nor has my family, in ways that many of my patients have who I’ve encountered.
I believe that the more that members of our physician and ancillary staff community resemble our patient community, the more we will get to that place of helping people feel welcome. I have asked myself over 10,000 times what would happen if I needed healthcare or my children needed healthcare and I went some place where I didn’t see anybody who looks like me or speaks my language? What would that experience have been, along with the stress of healthcare?”
As a program director, I also strongly believe that one of my primary roles is being an advocate for my group of 50 residents. Among my residents, diversity has always been verbalized as a top priority. We have ramped up our initiatives around diversity to honor the passion and the talents of my residents.
How is your residency program promoting diversity and recruiting a diverse group of residents?
Our program’s diversity committee was renamed the “JEDI” committee (Justice, Equity, Diversity & Inclusion) last year. The JEDI Committee has led a number of initiatives, including community outreach with high school students in local STEM pipeline programs, as well as procuring funding to help underrepresented minority medical students complete a month-long rotation with us.
In the last 3 years, we also overhauled our interview and recruitment practices. We now involve our residents in reviewing applications, which is unique. The residents need to establish their own community, and I want them to have a say in their community. Emergency medicine by its very nature is really hard work. One of the things that I prioritize to mitigate burnout is agency. Control over one’s own environment helps one to feel less out of control and less burned out.
We also implemented more equitable hiring practices. We train our resident and faculty evaluators before applications are released on the interview process and how to mitigate implicit bias when reviewing applications. After the applications are released, they are reviewed by the residents with attending oversight. Then I and a few educational division members conduct the final filter and select applicants to interview.
We ask our interviewers to focus on the four core values we are looking for in applicants:
- Commitment to BMC mission/capacity to care for underserved populations.
- Growth mindset: Values feedback, can persevere in the face of challenges.
- Resiliency: works well under pressure, in ambiguous circumstances, and/or while facing an overwhelming workload.
- Ability to assimilate into a team, to lead and follow example.
Board scores are reported but de-emphasized. My residents directed me to research* on how a heavy emphasis on standardized testing has led to inequities; some persons of color historically do worse on standardized tests, and that’s not a reflection of lower intelligence or less preparation as much as it is implicit bias.
We don’t have a board cutoff score. We acknowledge that not all of our applicants will have had access to the resources needed to get a stellar board score. A board score doesn’t define a good physician, a good healer, a good care provider. It’s just one of many data points. There is some data to suggest that USMLE Step score performance is at least somewhat predictive of board certification exam success. But as a competitive program, we believe strongly that our educational environment will meet the needs of our residents and get them to board certification.
Lastly, we assign structured questions to ask each applicant during the interview. An applicant who grew up in Utah but didn’t grow up in affluence said she would be in interviews in which somebody would say, “You’re from Utah. Where are your favorite places to ski?” She couldn’t afford to go to a Utah ski resort. Just that simple, free-flowing question from an otherwise well-intentioned faculty member was profoundly alienating for her.
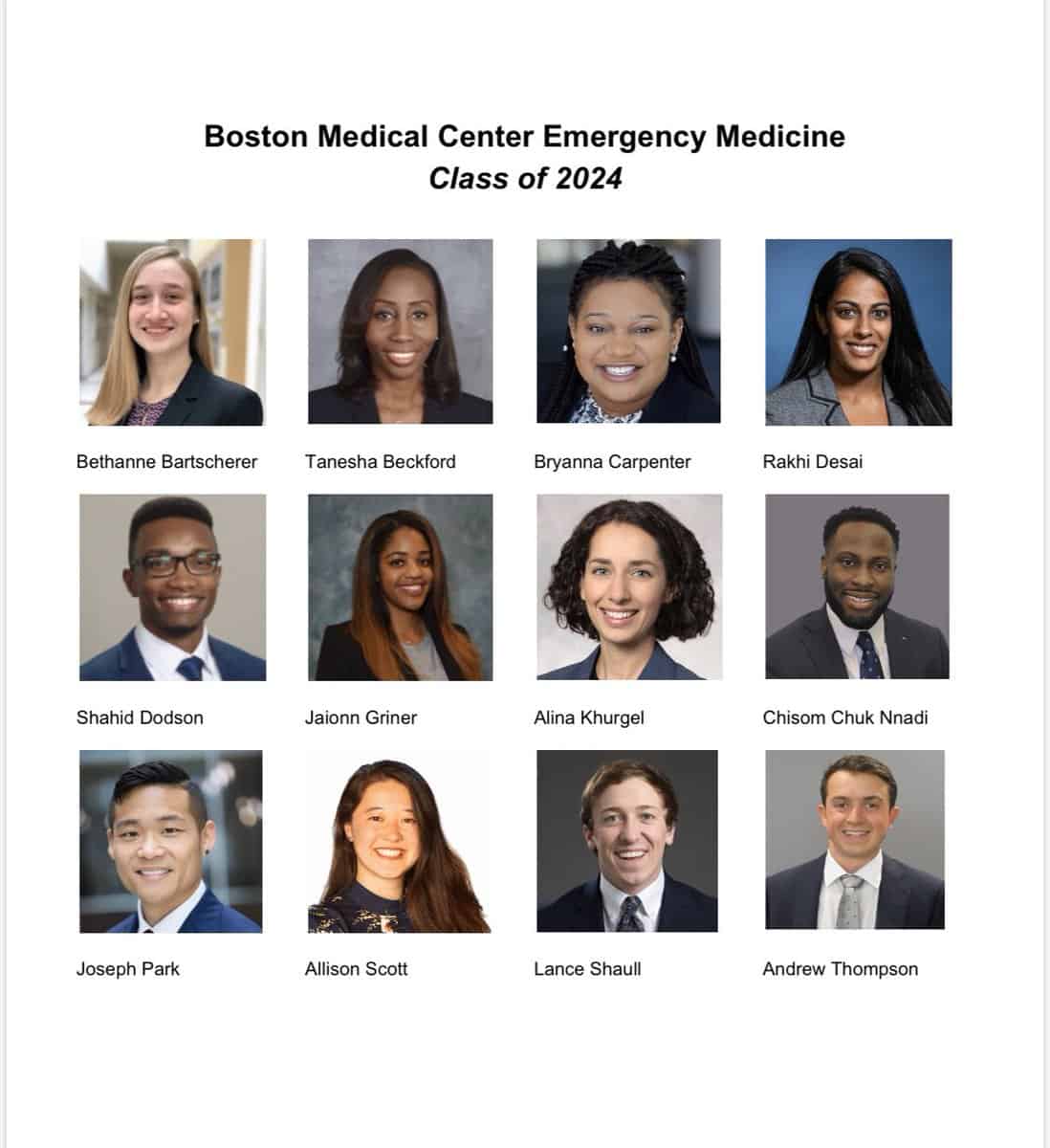
Our efforts are paying off. Although we have always had reasonable gender diversity, and diversity within the LGBTQ community, this year, our intern class increased in racial/ethnic diversity. Among the 12 members of the class of 2024, seven (58%) are female, six (50%) identify as underrepresented minority, and five (42%) identify as African American.
 We create a welcoming environment where our residents can learn to be a good doctor and feel respected and appreciated. Some of that is due to our very explicit ideals around diversity in the JEDI committee. BMC’s Department of Graduate Medical Education has put forth a strong effort toward diversity across departments as well.
We create a welcoming environment where our residents can learn to be a good doctor and feel respected and appreciated. Some of that is due to our very explicit ideals around diversity in the JEDI committee. BMC’s Department of Graduate Medical Education has put forth a strong effort toward diversity across departments as well.
In 2009, the Liaison Committee on Medical Education (LCME) made student diversity a requirement for medical school accreditation. It later made faculty diversity a requirement for accreditation. Despite these policy changes, medical schools/hospitals still fail to meet diversity standards for accreditation. What are your thoughts on why some institutions struggle and what can be done to help?
The issues are complicated and challenging. Even as of July 2020, within our residency, we haven’t achieved the full idea of diversity that I think many of us aspire to.
Addressing the issues surrounding the lack of diversity in medical schools and hospitals requires some uncomfortable conversations. If you are in a homogenous community that doesn’t have the diversity in line with these LCME ideals, perhaps you are not having those uncomfortable conversations.
I think some communities give diversity lip service, while others are really hoping to move in the right direction but aren’t having the right conversations, or they’re giving voice to a commitment to diversity but not saying it in a way that seems some combination of sincere or in touch with really what’s going on. I think there are some other factors too.
My humble opinion is that more work is needed to really talk about the issues and get those in authoritative positions in medical schools, in residency programs, to listen—really listen—and listen in the truest sense. I feel I still have some of that to do myself; I’m trying.
To encourage adherence to the LCME diversity standards for accreditation, the federal government can give incentives, in the form of more funding for DEI efforts or resident salaries, for institutions that achieve better student and faculty diversity. I believe that would start spreading conversations about diversity to places where they are not currently happening.
The difficult conversations about race happening all over the country have happened for generations at BMC. When I was a resident, I participated in a retreat run by Dr. Thea James, who showed us a video on diversity. I never forgot a phrase from an African American saying “Black people encounter closed doors where white people don’t even see the doorway.” I believe these conversations are helping all of us see more doorways. They are making an impact.


 PWeekly
PWeekly
