Cerebral microbleeds (CMBs) in patients with embolic stroke of undetermined source (ESUS) conferred increased risk of recurrent stroke, but did not appear to influence the effects of the oral anticoagulant rivaroxaban (Xarelto) on clinical outcomes, subgroup analysis of NAVIGATE ESUS trial data showed.
“We found no indication of interaction between the effects of rivaroxaban and CMBs, including multiple or strictly lobar CMBs, for the outcome of intracerebral hemorrhage,” reported Ashkan Shoamanesh, MD, of McMaster University in Canada, in JAMA Neurology. “Our results and the existing literature from randomized trials and recent meta-analyses do not support the clinical concern regarding antithrombotic therapy in patients with ischemic stroke and CMBs.”
NAVIGATE ESUS was a phase III study of 7,213 patients 50 or older with recent ESUS that compared rivaroxaban 15 mg daily with aspirin 100 mg daily for prevention of recurrent stroke. It found rivaroxaban was not superior to aspirin and was associated with a higher risk of bleeding, both cited as reasons for early termination of the study.
In this subgroup analysis, Shoamanesh and colleagues identified 3,699 patients with CMBs reported as present or absent on baseline MRI prior to randomization. CMBs were present in 395 patients.
CMBs were tied to an increased risk of recurrent stroke (HR 1.5, 95% CI 1.0-2.3), intracerebral hemorrhage (HR 4.2, 95% CI 1.3-13.9), and all-cause mortality (HR 2.1, 95% CI 1.1-4.3). Strictly lobar microbleeds were associated with a 2.5-fold risk of ischemic stroke (HR 2.3, 95% CI, 1.3-4.3).
There were no interactions between microbleeds and treatment assignments for recurrent stroke, ischemic stroke, or all-cause mortality. The risk of intracerebral hemorrhage on rivaroxaban was similar between persons with microbleeds (HR 3.1, 95% CI, 0.3-30.0) and without microbleeds (HR 3.0, 95% CI 0.6-14.7; interaction P>0.99).
“The present study could contribute to changing the mindset of clinicians,” observed Charlotte Cordonnier, MD, PhD, and Laurent Puy, MD, both of the University of Lille in France, in an accompanying editorial. “Because the presence of CMBs does not seem to modify the effect of rivaroxaban on clinical outcomes, their use in guiding anticoagulation therapy decision-making is then questionable.
“Current evidence does not justify avoiding antithrombotic medication in patients with stroke based solely on the presence of CMBs,” they wrote. “In patients at high risk of ischemic stroke, clinicians should stop worrying about a possible bleed and start a solid evidence-based prevention of future ischemic events.”
But the findings need careful interpretation, they added: “Can we extrapolate this information to other direct oral anticoagulants? Probably. Can we extrapolate these results to types of ischemic strokes other than ESUS? No, not yet.”
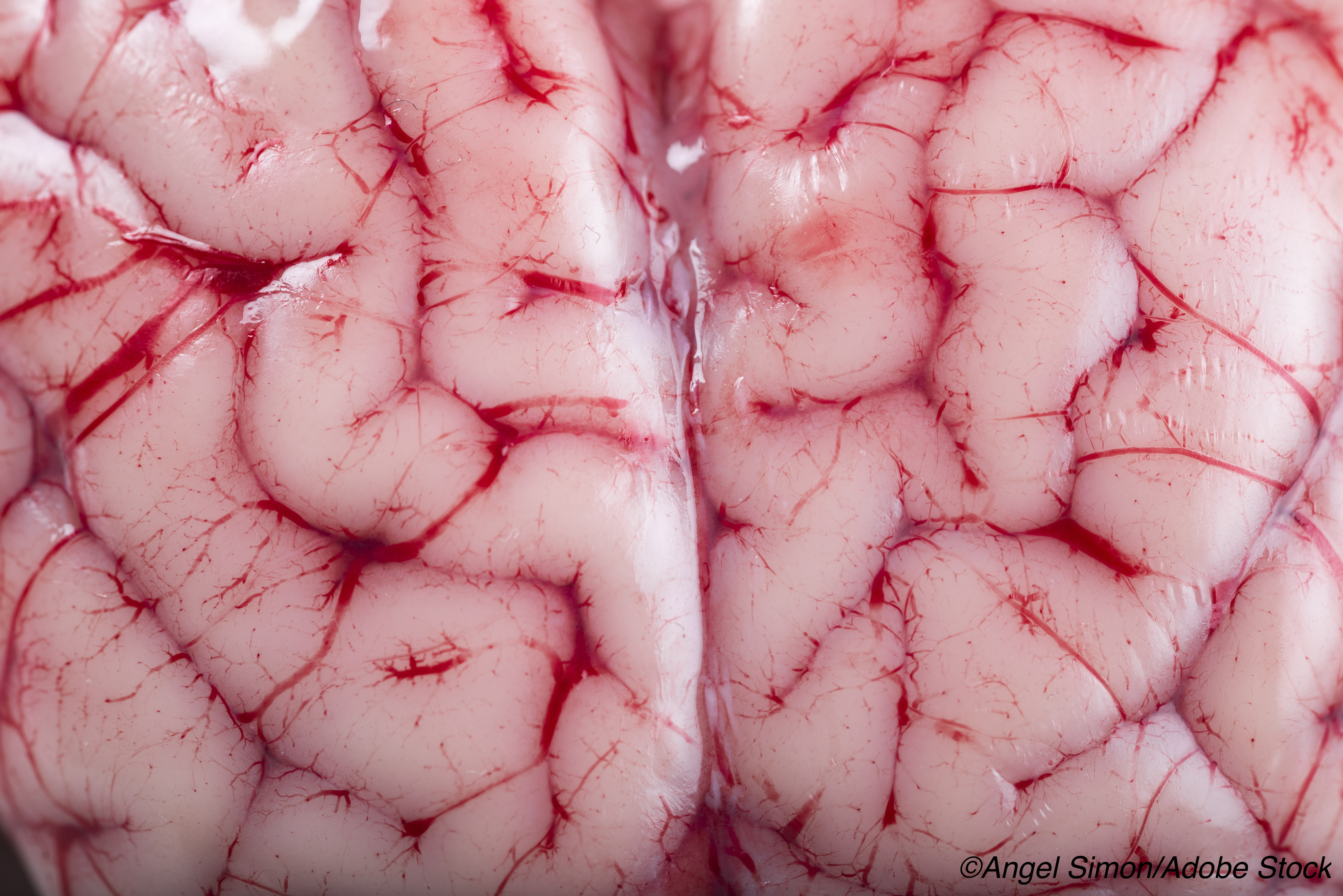
CMBs are found in healthy adults (5%), people with ischemic stroke (34%) and with non-traumatic intracerebral hemorrhage (60%). Their presence raises questions of added bleeding risk and whether antiplatelet agents or anticoagulants otherwise indicated for prevention of ischemic events should be avoided.
Recent research suggests that CMBs increase risk for ischemic stroke as well as bleeding, and that relative rates must be taken into account in specific patient subgroups. A 2018 observational study found for those with CMBs, the absolute rate of ischemic stroke (24.1 per 1,000 patient-years) was higher than symptomatic intracranial hemorrhage (9.8 per 1000 patient-years).
A 2019 pooled cohort analysis reported that for patients with recent ischemic stroke or transient ischemic attack, CMBs were associated with a greater relative hazard for intracranial hemorrhage than for ischemic stroke, but the absolute risk of ischemic stroke was higher than that of intracranial hemorrhage, regardless of cerebral microbleed presence, anatomical distribution, or burden.
“Patients with CMBs can be at risk of ICH but, in cohorts of ischemic strokes, they are at even greater risk of recurrent ischemic stroke,” Cordonnier and Puy noted.
In the present analysis, Shoamanesh and colleagues used data from NAVIGATE ESUS patients enrolled between December 2014 and September 2017 with median follow-up of 11 months. For patients with CMBs, mean age was 69.5, 61% were men (61%), and 51% were white. Of all with CMBs, 55% had strictly deep CMBs, and 26% strictly lobar CMBs.
CMB presence was independently associated with multi-territorial ESUS (OR 1.95, 95% CI 1.42-2.67). “This result deserves more attention,” the editorialists observed. “It may suggest that multi-territorial ESUS considered until now to be embolic could be associated with small vessel disease.”
Variables independently associated with CMBs were advancing age (OR per year 1.03), East Asian race/ethnicity (OR 1.57), hypertension (OR 2.20), multi-territorial infarcts (OR 1.95), chronic infarcts (OR 1.78), and occult intracerebral hemorrhage (OR 5.23).
Limitations included a lack of power to assess effects by CMB burden or distribution. Results were limited by trial eligibility criteria, possible selection bias during recruitment, and lack of MRI for CMB assessment in all NAVIGATE ESUS participants, which may limit generalizability.
-
Cerebral microbleeds (CMBs) in patients with embolic stroke of undetermined source (ESUS) conferred increased risk of recurrent stroke, but they did not appear to influence effects of rivaroxaban (Xarelto) on clinical outcomes, subgroup analysis of NAVIGATE ESUS trial data showed.
-
CMBs in patients with ESUS were also tied to increased risks in intracerebral hemorrhage and all-cause mortality. Strictly lobar microbleeds were associated with an increased risk of ischemic stroke.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was supported by Bayer AG and Janssen Research and Development.
Shoamanesh reported receiving grants and personal fees from Bayer AG, Bristol Myers Squibb, Daiichi-Sankyo, Servier Canada Inc, Janssen, and Bayer Canada and personal lecture and advisory board fees from Bayer AG, Bristol Myers Squibb, Boehringer Ingelheim, Servier Canada Inc, and Bayer Canada during the conduct of the study.
Cordonnier reported receiving personal fees from Boehringer Ingelheim during the conduct of the study and being a steering committee member of the AXIOMATIC-SSP trial sponsored by Bristol Myers Squibb.
Cat ID: 130
Topic ID: 82,130,130,38,748,192,925


