Recent reports have shown that the negative consequences of narcotic use are increasing, and diversion of these drugs for non-medical use is growing, with Americans consuming about 80% of the global opioid supply and 99% of the global hydrocodone supply. There has been an alarming rise in unintentional overdose deaths in the United States over the past decade due largely from increases in prescriptions of narcotics. It has been estimated that up to 20% of prescription drug abusers receive their narcotics from one physician prescriber, but a growing percentage obtain these medications by seeking multiple providers, a phenomenon dubbed “doctor shopping.”
Few studies, however, have looked at narcotic use in patients who have experienced orthopedic trauma. While some investigations have focused their attention on positive toxicology screenings at the time of admission after orthopedic trauma, there is limited research exploring the impact of postoperative doctor shopping and the role of orthopedic surgeons in this phenomenon. “It has been suspected that many orthopedic trauma patients may be at a higher risk for pre-injury narcotic use and doctor shopping,” says Hassan R. Mir, MD, MBA, FACS.
Exploring the Problem
Dr. Mir, Brent J. Morris, MD, and colleagues sought to identify the prevalence of patients who have had orthopedic traumas and were seeking multiple providers for narcotics after surgery in a study published in the Journal of Bone and Joint Surgery. For the analysis, the researchers reviewed prescription records for 151 adults who were admitted to an orthopedic unit over a 1-year period and assessed data on narcotic prescriptions obtained 3 months before and within 6 months after each orthopedic procedure. Patients were assigned to a single narcotic provider group, in which prescriptions were obtained only from the treating surgeon, or to a multiple provider group, in which prescriptions were received from treating surgeons and other providers.
Are your patients doctor shopping?
Click here to learn what patients are at highest risk for doctor shopping.
A Significant Issue
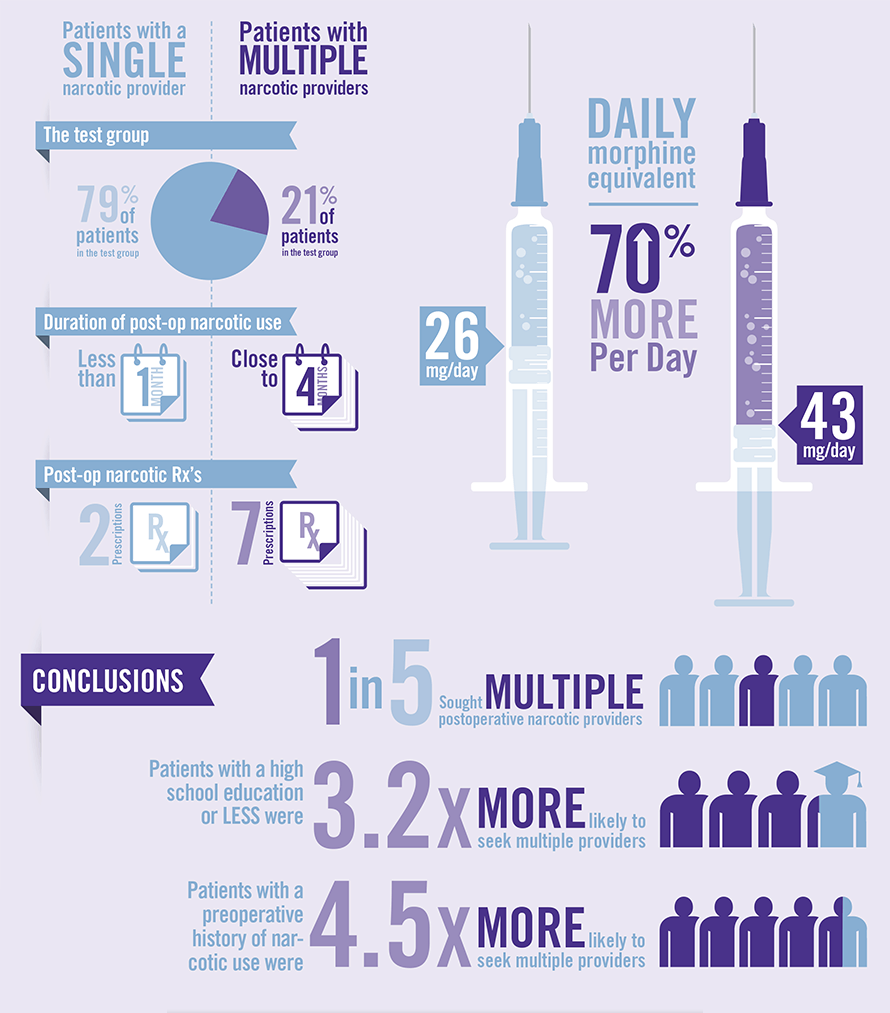
“We found that about one in five patients in our study were considered doctor shoppers and sought prescription pain medications from multiple providers,” says Dr. Morris. When compared with patients categorized into the single provider group, those who doctor shopped used narcotics four times longer. “Education and preoperative narcotic use were significant predictors of doctor shopping, even after controlling for alcohol use,” says Dr. Mir (Table 1). Patients with a high school education or less were 3.2 times more likely to seek multiple providers. Those with a history of preoperative narcotic use were 4.5 times more likely to seek multiple providers after their surgery.
Differences in outcomes were also compared between patients with a single provider and those with multiple providers (Table 2). When compared with patients receiving postoperative narcotics exclusively from their treating surgeon, doctor shoppers obtained significantly more postoperative narcotic prescriptions. The duration of postoperative narcotic use and the morphine equivalent doses per day were also significantly higher for doctor shoppers than for the single-provider group.
What Can Clinicians Do?
Although it is important to identify which patients are more likely to doctor shop, Dr. Morris says that this is often challenging for clinicians. “It’s difficult to tell if patients are likely to doctor shop for narcotics after they’ve undergone surgery,” he says. “Our study results suggest that we should consider less education and a history of using prescription narcotics as red flags for potential doctor shopping.”
Prescription drug monitoring programs are available in most states and collect data on controlled substances in order to deter diversion, narcotic abuse, and doctor shopping. However, not every state has active prescription drug monitoring programs, and only seven have laws in place requiring providers to use their state’s prescription drug monitoring database. Dr. Morris says that surgeons should utilize prescription drug monitoring databases, if possible, before prescribing narcotics so that they can check to see if patients have received these prescriptions from other providers in the past.
According to Dr. Mir, the study findings also highlight the importance of counseling patients about pain control. “While we strive for high patient satisfaction, patients should understand what can be reasonably expected regarding the use and effectiveness of pain medications after surgery,” he says. “We must prescribe these drugs with great care and vigilance to minimize risks of abuse, dependence, and narcotic-related adverse events. It’s important for doctors and patients to establish trust in each other and work together when discussing treatment plans and throughout follow up.”