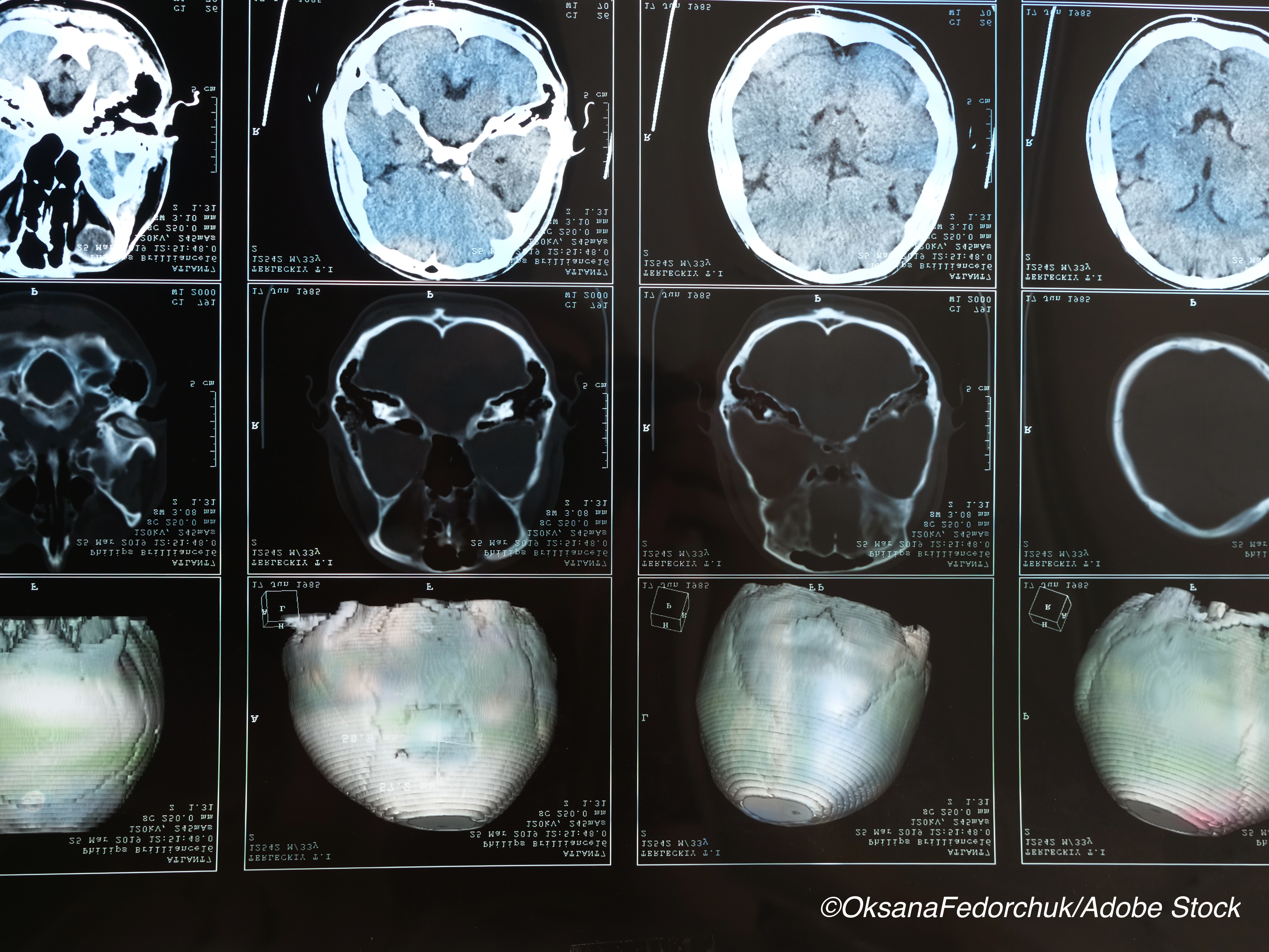
Early evidence of white matter injury detected with advanced magnetic resonance imaging (MRI) was associated with persistent symptoms in people with mild traumatic brain injury (TBI), according to results from a prospective study from Europe.
The multicenter study included 81 patients presenting for treatment within 24 hours of experiencing head trauma who received MRIs within 72 hours after injury and again two to three weeks later.
TBI patients showed declines in white matter volume on the second MRI that were not seen on initial imaging, and these findings suggest that “advanced MRI reveals potential neuroanatomical substrates of [mild TBI] in white matter and is most strongly associated with odds of recovery if performed within 72 hours, although future validation is required,” researcher Sophie Richter, MD, of the University of Cambridge, U.K., and colleagues wrote in JAMA Network Open.
The researchers also noted that their analysis, which also included 104 controls, is the largest to date in patients diagnosed with mild TBI who had serial MRIs within the first weeks after injury.
“Our data document the dynamic evolution of both conventional and advanced MRI (using diffuse tensor imaging), with the earlier point (<72 hours) showing potential prognostic value,” they wrote.
Ritcher and colleagues wrote that based on the level of consciousness on presentation, 70% to 90% of traumatic brain injuries are classified as mild, even though as many as half of these patients experience associated symptoms that last six months or longer.
“Although symptoms may be reduced by early intervention, the large numbers of patients with mild TBI prohibit unselected follow-up without overburdening the system,” they wrote. “Similarly, because many patients recover fully, trials of early interventions using unselected populations with mild TBI are underpowered. We therefore need ways to enrich populations for clinical follow-up and interventional trials.”
They noted that while conventional imaging (radiographic CT and structural MRI) does not typically differentiate between patients who do and do not develop persistent symptoms, advanced MRI, such as volumetric analysis and diffusion tensor imaging (DTI), shows promise “in detecting anatomical changes associated with outcome after mild TBI, such as traumatic axonal injury.”
In an effort to better understand the clinical benefits of advanced imaging in the management of people with mild TBIs, the researchers conducted a prospective multicenter study involving all eligible (n=81) patients in the Collaborative European NeuroTrauma Effectiveness Reearch in TBI (CENTER-TBI) study.
All patients underwent an initial MRI within 72 hours (MR1) and a second MRI within the following 31 days (MR2). Thirty-nine of the 81 patients underwent a third MRI (MR3) at three months.
Across the nine study sites, 12 MRI scanners each contributed six to 25 healthy volunteers of comparable age and sex who underwent imaging with the same protocol (n=104).
The median age of the patients included in the analysis was 45 years (interquartile range [IQR], 24-59; range, 14-85), and 57 (70.4%) were male. Structural sequences were available for all scans; diffusion tensor imaging data were available for 73 MR1 scans and 79 MR2 scans.
After adjustment for multiple comparisons between scans, visible lesions did not differ significantly, but cerebral white matter volume decreased (MR2:MR1 ratio, 0.98; 95% CI, 0.96-0.99) and ventricular volume increased (MR2:MR1 ratio, 1.06; 95% CI, 1.02-1.10).
Among the other study findings:
- White matter volume was within reference limits on MR1 scans (patient to control ratio, 0.99; 95% CI, 0.97-1.01) and reduced on MR2 scans (patient to control ratio, 0.97; 95% CI, 0.95-0.99).
- Symptoms, measured by standardized concussion questionnaire worsened in the progressive injury phenotype (median, +5.00; IQR, +2.00 to +5.00]), improved in the minimal change phenotype (median, −4.50; IQR, −9.25 to +1.75), and were variable in the pseudo-normalization phenotype (median, 0.00; IQR, −6.25 to +9.00) (P=0.02).
- Recovery was favorable for 33 of 65 patients (51%) and was more closely associated with MR1 than MR2 (area under the curve, 0.87 [95%CI, 0.78-0.96] vs 0.75 [95% CI, 0.62-0.87]; P=0.009).
“The reduction in white matter volume between MR1 and MR2 could either be ascribed to resolution of early edema or to late loss of white matter,” the researchers wrote. “Compared with controls, patients had similar volumes at MR1 but reduced volumes at MR2. This finding suggests that the reduction of white matter volume at MR2 (which persisted at MR3) did not represent resolution of edema but rather new, persistent, and potentially progressive pathology.”
In commentary published with the study, Elie Massaad, MD, of Massachusetts General Hospital, Boston, and colleagues wrote that the study by Richter et al provides further evidence that there is an association between structural changes detected on diffuse tensor imaging, including decreased fractional anisotropy and increased mean diffusivity, and the severity and persistence of symptoms.
But they noted that “it remains very challenging to determine the optimal timing and specific MRI sequences in the evaluation and management of mild TBI that could have the most revealing prognostic value.”
The study suggested that the earliest MRI was a better predictor of outcomes than later MRI, but the researchers noted that, because DTI within 72 hours of injury has been shown to be associated with an increase in fractional anisotropy and decrease in diffusivity, more research is needed to “determine the time course of edema that best manifests on imaging and with outcomes.”
“Future studies to explore the prognostic value of imaging biomarkers in mild TBI would benefit from larger sample size, external validation of the presented results, and incorporation of time-dependent and multiple sequences to enhance risk prediction of outcomes,” they wrote.
“Given the large spectrum of mild TBI and the scarcity of imaging data available for research, future efforts should focus on making available sufficiently large, curated, and standardized imaging libraries to allow for more robust analysis of imaging features to better understand their role in diagnosis and prognosis of mild TBI.”
-
Early evidence of white matter injury detected with advanced magnetic resonance imaging was associated with persistent symptoms in people with mild traumatic brain injury.
-
White matter volume and integrity evolved between the first MRI taken within 72 hours of injury and the second, taken two to three weeks later.
Salynn Boyles, Contributing Writer, BreakingMED™
Funding for this study was provided by the European Comission, Hannelore Kohl Stiftung, NeuroTraumaSciences, LLC, and Integra Neurosciences.
Researcher Sophie Richter reported receiving personal fees from Wellcome Trust during the conduct of the study. Researcher Virginia Newcombe reported receiving grants from F. Hoffman-LaRoche Ltd and personal fees from Neurodiem Honorarium.
Cat ID: 474
Topic ID: 82,474,254,730,474,192,925,481


