1. Patients with large cerebral infarctions receiving endovascular therapy with medical care had better functional outcomes than patients receiving medical care alone.
2. A significantly greater proportion of patients receiving endovascular therapy experienced intracranial hemorrhage than patients treated with medical care alone.
Evidence Rating Level: 1 (Excellent)
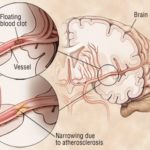
Study Rundown: Small acute ischemic strokes with an Alberta Stroke Program Early Computed Tomographic Score (ASPECTS) greater than 6 are often treated with endovascular therapy; however, its efficacy is unknown in larger strokes (ASPECTS score 3 to 5). To investigate whether endovascular therapy improved functional outcomes in these patients, 203 patients in Japan with large ischemic strokes with ASPECTS scores 3 to 5 were randomized in a 1:1 ratio to either received endovascular therapy with medical care or medical care alone. The primary outcome was to assess improvement in functional outcomes as measured by the modified Rankin scale. The results found that a greater proportion of patients receiving endovascular therapy had a score of 0-3 on the modified Rankin scale 90 days after stroke onset compared to patients receiving medical care only. Patients receiving endovascular therapy also showed improvements in the National Institutes of Health Stroke Score (NIHSS), but also a significantly higher incidence of intracranial hemorrhage. No differences were found in other safety outcomes including recurrence of cerebral infarction, the requirement of decompressive craniotomy, or death. Together, this study supports the use of endovascular therapy in patients with a large acute ischemic stroke to improve functional outcomes. Limitations of this study include a potential lack of generalization between Japanese patients and the international population, a selection bias for patients who would benefit from endovascular therapy, and limited use of alteplase to assist outcomes in both groups.
Click to read the study in NEJM
Relevant Reading: Triage imaging and outcome measures for large core stroke thrombectomy – a systematic review and meta-analysis
In-Depth [randomized controlled trial]: In this multi-center, open-label randomized control trial named RESCUE-Japan LIMIT, 203 patients in Japan diagnosed with acute ischemic stroke by occlusion of a cerebral artery, at least 6 on the National Institutes of Health Stroke Scale (NIHSS) and low (0-1) modified Rankin score, and an Alberta Stroke Program Early Computed Tomographic Score (ASPECTS) between 3-5 upon admission were enrolled. Patients were randomized in a 1:1 manner to either received endovascular therapy (such as aspiration catheter, balloon angioplasty) in addition to standard medical care, or only received medical care alone. Alteplase was administered where necessary in both groups. The primary measured outcome was the proportion of patients with a modified Rankin score between 0 and 3, 90 days after the incidence of stroke. Secondary outcomes measured improvements in the modified Rankin score and improvement in stroke severity as measured by the NIHSS. The study also measured safety outcomes including symptomatic intracranial hemorrhage or recurrence of ischemic stroke. The results of the study found that 31.0% of patients receiving endovascular therapy achieved a 0-3 modified Ranking score, compared to 12.7% in the control group (relative risk [RR], 2.43; 95% confidence interval [CI], 1.35-4.37; P=0.002). The same trend was observed when assessing patients with an NIHSS score less than 6 with 31.0% in the endovascular group compared to 8.8% in the medical care group (RR, 3.51; 95% CI, 1.76-7). However, a greater proportion of patients receiving endovascular therapy (58.0%) also experienced intracranial hemorrhage compared to the control group (31.4%) (RR, 1.85; 95% CI, 1.33 -2.58; P<0.001). No differences were found in the other safety outcome measures. Taken together, this study supports the use of endovascular therapy in patients with acute ischemic stroke with an ASPECTS score between 3-5 in improving functional outcomes in this population.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.