1. Fractional flow reserve (FFR) guidance for percutaneous coronary intervention (PCI) was non-inferior to intravascular ultrasonography (IVUS) guidance.
2. Patient-reported outcomes for the use of FFR guidance or IVUS guidance were similar.
Evidence Rating Level: 1 (Excellent)
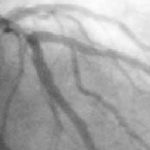
Study Rundown: For patients with coronary artery disease (CAD), the degree of luminal narrowing, plaque burden, and physiologic significance serve as prognostic indicators. IVUS is a commonly used adjunctive technique to provide detailed anatomical information about the lumen, vessel, and plaque, and can guide the PCI procedure to improve stent placement and minimize stent-related complications. Recently, IVUS-guided PCI has been shown to improve clinical outcomes when compared with angiography-guided PCI. FFR is an invasive physiologic index that can be used to determine whether a stenosis is causing ischemia, and previous trials have also demonstrated that FFR-guided PCI is associated with fewer clinical events than angiography-guided PCI. However, there is a gap in knowledge as to understanding the difference between IVUS and FFR-guided PCI with respect to clinical outcomes. Overall, this study found that in patients with intermediate coronary stenosis, FFR guidance was non-inferior to IVUS guidance with respect to death, myocardial infarction, or any revascularization at 24 months after the original procedure. This study was limited as it included low-risk patients in the trial population and operating physicians were aware of the trial-group assignments. Nevertheless, the findings are significant, as they demonstrate that FFR-guided PCI provides similar benefits and clinical outcomes as IVUS-guided PCI, with FFR-guided PCI also leading to a lower frequency of stent implantation.
Click to read the study in NEJM
Relevant Reading: Five-Year Outcomes with PCI Guided by Fractional Flow Reserve
In-Depth [randomized controlled trial]: This prospective, randomized, open-label multinational trial was conducted at 18 sites in Korea and China. Patients who were 19 years or older with de novo intermediate stenosis (40-70%) in a target vessel measuring at least 2.5mm by visual estimation on coronary angiogram were eligible for the study. Patients with a noncardiac coexisting illness and life expectancy of less than 2 years, a target lesion located in the left main coronary artery or in a coronary artery bypass graft, or an increased bleeding risk were excluded from the study. Patients were randomly assigned to undergo FFR or IVUS-guided procedures. The primary outcome measured was a composite of death, myocardial infarction, or any revascularization at 24 months after randomization. Outcomes in the primary analysis were assessed via the Cox proportional-hazards model and Kaplan-Meier method with scaled Schoenfeld residuals over time at a level of 0.05. Based on the primary analysis, the frequency of PCI among all target vessels was 33.2% in the FFR group and 58.4% in the IVUS group. A primary-outcome event at 24 months occurred in 8.1% of the patients in the FFR group and in 8.5% of the patients in the IVUS group (absolute difference, −0.4%; upper boundary of the one-sided; 97.5% Confidence Interval, 2.2%; p=0.01 for noninferiority). Patient-reported outcomes as reported on the Seattle Angina Questionnaire were similar in the two groups. Overall, this study demonstrates that FFR guidance is non-inferior to IVUS guidance with respect to outcomes of death, myocardial infarction, or revascularization at 24 months in patients with intermediate stenosis.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.