Although they are beneficial in reducing inflammation, glucocorticoids have been linked with many well-known adverse effects, and their use often elicits fierce debate.
Glucocorticoids (GCs) have shown great value due to their anti-inflammatory and immunosuppressive properties. They have been widely used to treat diseases such as rheumatoid arthritis (RA), vasculitis, lupus, and inflammatory myopathies. There is, however, debate among practitioners regarding the benefit-risk profile of GCs, according to Frank Buttgereit, MD, who notes that the potential side effect of GCs is of great concern.
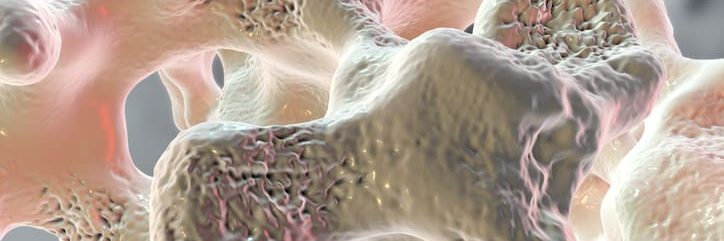
For a study published in the Annals of Rheumatic Diseases, Dr. Buttgereit and colleagues analyzed the impact of variables that influence osteoporosis in patients with inflammatory rheumatic and musculoskeletal diseases (iRMDs) who are on GCs. “In addition to their beneficial effects on reducing inflammation, GCs are also associated with many well-known adverse effects. Their use often elicits fierce debates on the benefit-risk profile,” Dr. Buttgereit explains.
In 2015, the Inflammatory and Rheumatic and Musculoskeletal Diseases and Glucocorticoid-Induced Osteoporosis (Rh-GIOP) open cohort study addressed how GC treatment is modified by other factors. These include inflammatory activity, age, regular exercise, menopausal status, vitamin D levels, and current therapy of both the underlying disease as well as osteoporosis (Figure).
Bone Mineral Density Measured at Lumbar Spine and Femur
The final analysis for the study included 1,066 patients aged 62 (±13); 76% were women and of those women, 89% were postmenopausal. Patients with the following iRMDs were included in the study: RA, connective tissue diseases, vasculitides, and spondyloarthritides (including psoriatic arthritis).
The study participants had their bone mineral density (BMD) measured at the lumbar spine and bilateral proximal femur by dual X-ray absorptiometry (DXA). The result of these measurements is expressed as T-scores with < −1.0 to > −2.5 scores classified as osteopenic and ≤ – 2.5 scores classified as osteoporotic.
GCs were taken by 75% of participants with a median daily dose of 5 mg. Twenty-two percent of participants had osteoporosis (ie, the lowest measured T-scores), and osteopenia was noted in 49% of patients.
Four categories of GC dosing were outlined: no GC, >0 mg/day to <5 mg/day, 5.0−7.5 mg/day, and >7.5 mg/day. The researchers observed no differential effects on the participating patients’ T-scores if they were in the category of no GC and the category of >0 mg/day to <5 mg/day. They did, however, note negative effects in the category of >7.5 mg/day.
Patients With the Most Active Disease More Likely to Receive High GC Doses
GC doses of >5mg/day also had a significant negative association in patients with RA with these patients showing the lowest overall T-score (−0.49) and lumbar spine score (−0.49), together with the following factors: age, menopause, BMI, alkaline phosphate, biophosphonates, disease duration, denosumab, and male sex. Similar results were found in patients taking GCs at >7.5 mg/day.
In the interaction analysis of GC with disease activity, T-scores appeared to only be negatively impacted in patients who had a moderate or high disease activity and current dosing of GCs at >7.5 mg/day. No negative effects were seen in those patients taking 5 mg/day regardless of the disease activity level.
Dr. Buttgereit expressed concern with framing the results of the study properly. “Observational research in GC, including our research here, is highly susceptible to confounding/bias by indication,” he says. “In other words, we know that active inflammation itself deteriorates bone health, and patients with the most active disease are precisely the patients most likely to be treated with high doses of GCs.”


 Martta Kelly
Martta Kelly