For a study, the basal ganglia and a cerebello-thalamocortical circuit were both involved in the pathogenesis of Parkinson’s disease (PD) tremor. It was unknown how these circuits produced tremor rhythm and amplitude, or whether these processes were influenced by tremor phenotypic. As per the previous research, researchers suggested that the cerebellum had a role in postural tremor in Parkinson’s disease. However, distinct forms of postural tremor (re-emergent or pure postural tremor) were included in the study, and region-specific effects on tremor amplitude were not examined. Researchers compared the function of the motor cortex (M1) and cerebellum in creating PD rest tremor rhythm versus amplitude to re-emergent tremor.
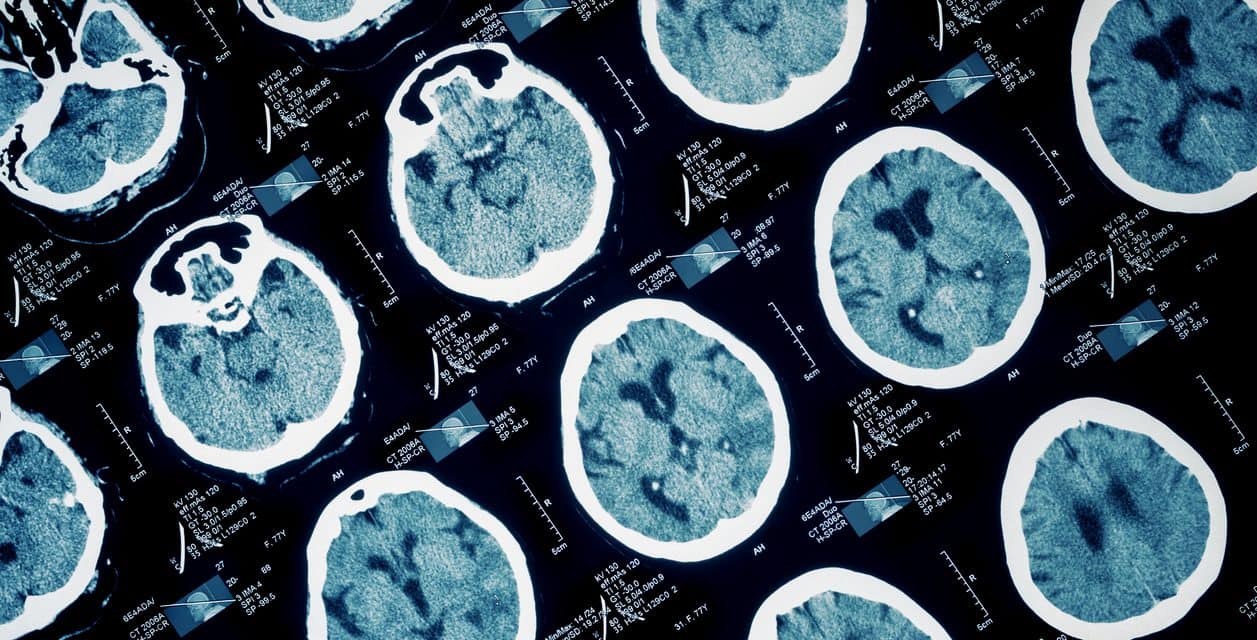
In 14 patients with PD, researchers investigated the impact of single-pulse transcranial magnetic stimulation (TMS) on tremor rhythm (tremor reset index [TRI]) and tremor power (electromyography).
All patients reported rest tremor and electrophysiologically verified re-emergent tremor, with wrist extension suppressing tremor amplitude for up to 3000 milliseconds (F1,20=11.7, P<0.001; part.η2=0.47). Cerebellum-TMS effectively reset re-emergent tremor but not rest tremor (t13=2.1, P=0.026; Cohen’s d=0.57; TRI vs. 0 [re-emergent tremor: t13=3.0, P=0.010; rest tremor: t13=1.0, P=0.33]). The TRI after cerebellum-TMS decreased with consecutive tremor bursts (1–5 following TMS) in re-emergent tremor, indicating temporary resetting (time: F4,52=3.61, P=0.011; part.η2=0.22; Table S2). M1-TMS decreased tremor power in both rest and re-emergent tremor (site-time interaction: F8,104=8.77, P<0.001; part part.η2=0.40 [no 3-way interaction with tremor type]). M1-TMS decreased tremor power in both tremor types by up to 1500 milliseconds (rest tremor, time: F8,104=8.17, P<0.001; part part.η2=0.39; re-emergent tremor, time: F8,104=13.24, P<0.001, part.2=0.50), whereas cerebellum-TMS had no effect.
Reference:movementdisorders.onlinelibrary.wiley.com/doi/10.1002/mds.28603