While Pott’s puffy tumor remains under-recognized and misdiagnosed, reported cases are increasing with improved understanding of the disease and better imaging.
Pott’s puffy tumor is often under-recognized and misdiagnosed because of its variable clinical presentation and may be inadequately treated due to a lack of guidance in the literature, according to a comprehensive review published in the American Journal of Otolaryngology.
“One of my coauthors, Dr. Khalili, and I were discussing the disease process and the frequency,” David M. Poetker, MA, MD, explains. “We looked at the literature and there really were no good articles that summarized what clinicians need to know about Pott’s puffy tumor.”
Pott’s puffy tumor is a rare disease process characterized by osteomyelitis of the frontal bone with subperiosteal abscess formation. Patients often present with localized forehead edema, usually due to frontal sinus disease. Since it was first recognized in the 18th century, approximately 300 cases have been reported in the literature, most in the last decade.
“I think more cases have been reported recently due to the increased understanding of the disease, the better imaging available, and the ease of reviewing the literature and publishing today compared with 30-40 years ago,” Dr Poetker said.
The review included 216 articles describing 318 patients with Pott’s puffy tumor and 3 cases treated at their institution, yielding data for 321 patients (age, 8 months to 90 years; mean age, 29.1 years). Articles included in the analysis were primarily case series or case reports.
Epidemiology, Etiology, and Signs & Symptoms
The incidence of Pott’s puffy tumor remains unclear because of its rarity. It is thought to be somewhat more common in pediatric patients; however, the cases included in the comprehensive review showed a slight predominance in the adult population over the past decade. The authors note that this may be indicative of a relative increase in cases in the adult population, or an artifact of better diagnostic methods and greater awareness of Pott’s puffy tumor among adults.
Most cases of Pott’s puffy tumor were associated with acute or chronic rhinosinusitis (82.9%). Other common etiologies included a history of direct trauma to the forehead (17.1%), odontogenic disease (11.5%), intranasal substance abuse (6.5%), diabetes (5.6%), and rheumatologic disorders (2.5%). In 4% of cases, the etiology was unknown.
Although the clinical presentation of Pott’s puffy tumor varied, forehead swelling was common, observed in almost 80% of patients. Other frequent findings included frontal headache (56.7%), fever (35.5%), periorbital edema or erythema (23.4%), and purulent or non-purulent rhinorrhea (19.3%). Rarely, patients had neurological outcomes, including seizures, meningeal signs, or focal neurological signs (10.6%). Vision changes were reported in 8.7% of patients.
In most cases, the signs and symptoms evolved over the course of a few days to weeks. Periodic forehead swelling occurring over several months to years was reported, but was uncommon. Before the onset of the hallmark signs and symptoms of Pott’s puffy tumor, patients reported facial pain or pressure, nasal congestion, and rhinorrhea 4 to 5 weeks prior to presentation.
Diagnosing & Treating Pott’s Puffy Tumor
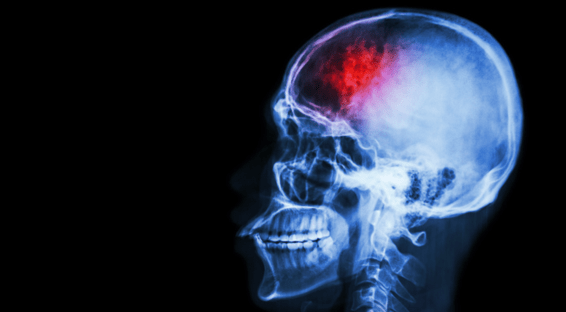
Radiographic imaging is essential to ensure rapid diagnosis and treatment, and the authors note that “imaging should not be delayed, as it can potentiate outcomes and prognosis.” In the current review, most were evaluated with CT alone (60.8%) or with CT plus MRI (32.9%). Use of standard radiography and ultrasonography were uncommon, performed in 3.8% and 1.3% of patients, respectively.
Microbiology and laboratory workups revealed most infections to be polymicrobial with an anaerobic-predominant microbiome. The most frequent causative organisms included Streptococcus (35.5%), Staphylococcus (21.2%), Fusobacterium (5.3%), Pseudomonas (3.4%), and Prevotella (2.2%).
Treatment includes broad-spectrum antibiotics and surgical intervention, with surgical interventions increasing in the last two decades (Figure). Most patients were treated with a combined endoscopic and open approach (37.7%), with external drainage in 31.8% of patients and endoscopic sinus surgery alone in 27.7% of patients.
“These patients need to be seen by a rhinologist who can adequately drain the frontal sinus as well as ensure patency of the drainage. The disease process recurs if the frontal sinus is not adequately opened,” Dr Poetker said. He encouraged primary care providers and ED physicians to become familiar with the disease process of Pott’s puffy tumors. “External drainage can lead to fistulas and chronic drainage from the forehead skin,” he says.


 Julia Ernst
Julia Ernst