1. This cohort study based on a nationwide Sweden registry demonstrated that among adult patients with a recent acute myocardial infarction (MI) who were discharged on antithrombotic therapy, ischemic events were more common and associated with a higher risk of 1-year mortality compared to bleeding events.
2. Physicians should consider the difference in the risk of ischemic versus bleeding events with the risk of mortality when developing personalized antithrombotic therapy management plans for patients post-acute MI
Evidence Rating Level: 2 (Good)
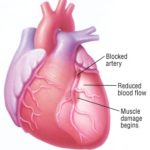
Study Rundown: Patients with a recent acute myocardial infarction (MI) are often started on antiplatelet and antithrombotic treatment to reduce the risk of recurrent ischemic events. However, this comes at the expense of increasing the risk of bleeding; therefore, guidelines recommend creating individualized antithrombotic therapy based on a patient’s ischemic and bleeding risk. This cohort study using nationwide registers in Sweden examined the association of ischemic and bleeding events with the risk of 1-year mortality in patients with a recent acute MI who was initiated on antithrombotic therapy. Adult patients with acute MI who were enrolled in the registry from January 1, 1997, to December 31, 2017, and were discharged alive with antithrombotic therapy were included. The primary outcome was the incidence of a first ischemic event or bleeding event within the first year of discharge. More patients experienced a first ischemic event (incidence rate: 5.7 events per 100 person-years) than a first bleeding event (incidence rate: 4.8 events per 100 person-years) within 365 days of discharge. Upon comparison of 1-year mortality risk, those who had an ischemic event (aHR: 4.16 [95% CI: 3.91-4.43]) or a bleeding event (aHR: 3.43 [95% CI: 3.17-3.71]) had a higher risk of death compared to those without such event. Additionally, an ischemic event was associated with a significantly greater mortality risk than a bleeding event (aHR: 1.27 [95% CI: 1.15-1.40]). After adjustment for smoking status, hemoglobin, and renal function, mortality risks did not significantly change. Furthermore, the relative mortality risk associated with bleeding and ischemic events did not significantly change when comparing data to the previous two decades (2001-2011 and 1997-2000). Overall, this nationwide cohort study in Sweden demonstrated that patients with a recent MI had a higher risk of an ischemic event than a bleeding event and that an ischemic event was associated with greater mortality risk. These findings suggest that a personalized management plan post-MI for patients may require more weight on limiting ischemic events rather than bleeding events. One limitation of this study, however, is that it only investigated the risk of mortality within one year; future studies should compare the long-term risk of ischemic versus bleeding events, given that patients are typically on antiplatelet and/or antithrombotic therapy for many years post-MI.
Click to read the study in JAMA
Relevant Reading: Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.