1. Event-free survival and median overall survival were significantly longer in the combination group
2. Febrile neutropenia and infections occurred less frequently in the combination group, while neutropenia and bleeding had a higher occurrence
Evidence Rating Level: 1 (Excellent)
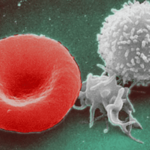
Study Rundown: Certain patients, especially of older age, with acute myeloid leukemia are considered unfit to receive induction chemotherapy and are more limited in their treatment options. This study explored the use of (an inhibitor of mutant isocitrate dehydrogenase 1 (IDH1)) and azacitidine (a DNA methyltransferase inhibitor) on newly diagnosed IDH1-mutated acute myeloid leukemia patients who were ineligible for induction chemotherapy. Patients were assigned to receive either ivosidenib and azacitidine or placebo and azacitidine. Event free survival (EFS) and median overall survival (OS) were significantly longer in the combination group. A higher proportion of patients in the combination group had a complete remission and transfusion independence. Health-related quality of life scores were higher in the combination group. When indirectly compared to venetoclax plus azacitidine, the ivosidenib and azacitidine had a longer EFS and higher proportion of patients with complete remission, though there is caution in cross-trial comparisons. Adverse events that occurred were expected of acute leukemia treatments. Adverse events grade 3 or higher occurred in nearly all patients and were comparable across both groups. Febrile neutropenia and infections occurred less frequently in the combination group, while neutropenia and bleeding occurred more frequently. Limitations to this study include its small sample size and its indirect comparison to other first-line therapies. The strength of this study is that it provides a treatment option to IDH1-mutated acute myeloid leukemia patients ineligible for induction chemotherapy. Overall, this study showed the clinical benefits of ivosidenib and azacitidine in IDH1-mutated acute myeloid leukemia and is a viable treatment option.
Click to read the study in NEJM
Relevant Reading: Acute myeloid leukemia with IDH1 and IDH2 mutations: 2021 treatment algorithm
In-Depth [randomized control trial]: This global, phase III trial randomly assigned 146 patients with newly diagnosed IDH1-mutated acute myeloid leukemia patients who were ineligible for induction chemotherapy; 72 in the ivosidenib and azacitidine group and 74 in the placebo and azacitidine. EFS was significantly longer in the combination group (hazard ratio [HR] for treatment failure, relapse from remission, or death, 0.33; 95% confidence interval [CI], 0.16 to 0.69; P=0.002). Median OS was 24.0 months for the combination group and 7.9 months for the placebo group (HR for death, 0.44; 95% CI, 0.27 to 0.73; P=0.001). Complete remission occurred in 47% of patients in the combination group (95% CI, 35 to 59) and in 15% of patients in the placebo group (95% CI, 8 to 25). Transfusion independence was reached in 46% of patients in the combination group, compared to 18% in the placebo group (P=0.006). When indirectly compared to venetoclax plus azacitidine, ivosidenib plus azacitidine had a 6.5 month increase in median OS and 18.9% increase in complete remissions. Adverse events of grades 3 or higher occurred in 93% of patients in the combination group and 95% in the placebo group. Main differences in occurrence of adverse events of any grade were observed with febrile neutropenia (combination group 28%, placebo group 34%), infections (28% and 49%), neutropenia (28% and 16%), bleeding (41% and 29%), and differentiation syndrome (14% and 8%). Overall, ivosidenib and azacitidine therapy increased EFS, median OS, quality of life, transfusion independence, and incidence of complete remission compared to placebo and azacitidine.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.