1. At a 4-year follow-up for relapsed or refractory multiple myeloma (RRMM) patients treated with LCAR-B38M CAR-T cell therapy, 37.8% had passed away from disease progression, 87.8% achieved at least a partial response, 73.0% achieved a complete response, and 21.6% had a complete response with no disease progression.
2. The most prevalent long-term adverse event (AE) was viral infection from B cell aplasia (5.41% of patients), as well as development of other primary non-hematological malignancies (5.41%), although all patients had at least one AE occur within 100 days post-infusion.
Evidence Rating Level: 2 (Good)
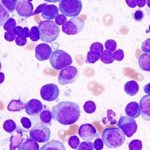
Study Rundown: Multiple myeloma (MM) is a malignancy of plasma cells that has been difficult to treat with chemotherapies, with a 5-year overall survival (OS) of lower than 30%. Even with novel therapies that have improved survival, such as proteasome inhibitors (PIs) and immunomodulatory drugs (IMiDs), drug resistance and relapse are issues that still persist. Chimeric antigen receptor (CAR)-T cell therapy is a potential treatment for B cell malignancies, which eliminates cancer cells through its interaction with tumour surface antigens, including B cell maturation antigen (BCMA), a glycoprotein necessary for plasma cell survival and uniquely expressed in B-cells. A first-in-human trial of CAR-T targeting BCMA was done in China, known as the LEGEND-2 study. The therapy used was known as LCAR-B38M, which comprised of two BCMA-targeting antibodies. Although the study was limited by not comparing LCAR-B38M to other standard treatments for MM, this study specifically enrolled patients with relapsed or refractory multiple myeloma (RRMM), who had previously undergone standard treatments including PIs, IMiDs, and stem cell transplant. LEGEND-2 demonstrated an overall response rate (ORR) of 88%, and with a 2-year follow-up, and a median progression-free survival (PFS) of 19.9 months or 18.0 months, depending on the site. A separate study, known as CARTITUDE-1, found an ORR of 98%, with median PFS and overall survival (OS) not reached at 22-months follow-up. The current study is a 4-year follow-up of the participants in LEGEND-2, the longest follow-up for CAR-T therapy for RRMM. The results showed that 73.0% had a complete response (CR) to the therapy, median duration of response (DOR) was 23.3 months, median PFS was 18.0 months, and median OS was not reached. Furthermore, most adverse events (AEs) occurred acutely after LCAR-B38M infusion, such as cytokine release syndrome (CRS), with B cell aplasia being the most prevalent chronic AE, associated with 5.41% of patients having treatable viral infections.
Click here to read the study in the BMC Journal of Hematology & Oncology
Relevant Reading: Exploratory trial of a biepitopic CAR T-targeting B cell maturation antigen in relapsed/refractory multiple myeloma
In depth [prospective cohort]: The study population consisted of 74 patients with RRMM between the ages of 18 and 80 years, with a median number of 3 prior therapies (range 1-9). Depending on the site, lymphodepletion was achieved with cyclophosphamide or cyclophosphamide plus fludarabine, and the LCAR-B38M CAR-T cells were given in three separate infusions (n=65) or one infusion (n=9), with a median dose of 0.513×106 cells/kg. The ORR was defined as the percentage of patients achieving a partial response or better, as defined by the International Myeloma Working Group consensus recommendations. As well, adverse event (AE) grades were assigned using the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.03. Data on safety assessed through rates of CRS, virus infection after infusion, and occurrence of other primary non-hematological malignancies. The median follow-up was 47.8 months, at which point 34 patients had died, 28 (37.8%) from disease progression, and 39 (52.7%) patients remained on the study. The study found that all patients experienced an acute AE in the first 100 days following infusion, with 60.8% experiencing a Grade 3 or higher acute AE, with the highest being leukopenia (25.7%), thrombocytopenia (18.9%), and AST elevation (20.3%). As well, CRS occurred for 91.9% of patients (8.1% grade 3 severity, 1 grade 5 severity, 1 fatality) with a median onset of 9 days post-infusion. The most prevalent chronic AE was B cell aplasia: 3 patients had herpes zoster virus activation at 7, 26, and 46 months post-infusion respectively, whereas 1 patient had hepatitis B infection at 7 months respectively, with all activations being treatable with antiviral drugs. As well, 4 patients had occurrence of other primary non-hematological malignancies, including lung cancer at 8 and 32 months post-infusion, esophageal cancer at 15 months, and cervical cancer at 8 months. With regards to efficacy, 73.0% of patients achieved CR, the ORR was 87.8%, and the median time for initial and best response were 1.02 (range 0.4-3.5) and 3.32 (range 0.43-28.52) months respectively. The median DOR was 23.26 months (95% CI 13.04-32.69) and the median PFS was 18.04 months (95% CI 10.61-25.56). At 4-year follow-up, 16 of the 39 surviving patients (21.6% of all enrolled participants) had CR with no disease progression, with one patient followed up at 60 months found to be disease-free, and the last death occurring at 36.14 months follow-up. The median OS was not yet reached, but the 24-month OS rate was 63.4%. Furthermore, 43 patients (58.1%) subsequently developed progressive disease (PD). 21 of these patients (28.4%) survived, with some being re-treated with CAR-T in a separate study, with a PI, or with a therapy they previously were not treated with. Overall, this study demonstrated the promise of LCAR-B38M CAR-T cell therapy for RRMM, with limited chronic adverse events.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.