 Among patients with type 2 diabetes and established heart disease undergoing revascularization, elevated low-density lipoprotein cholesterol (≥100 mg/dL) was associated with an increased risk for major adverse cardiac or cerebrovascular events (MACCE) 1 year later in a pooled analysis of 3 large clinical trials.
Among patients with type 2 diabetes and established heart disease undergoing revascularization, elevated low-density lipoprotein cholesterol (≥100 mg/dL) was associated with an increased risk for major adverse cardiac or cerebrovascular events (MACCE) 1 year later in a pooled analysis of 3 large clinical trials.
When compared with optimal medical therapy (OMT) alone, patients randomized to coronary artery bypass grafting (GABG) in the trials had lower rates of MACCE at any 1-year LDL cholesterol level, while patients who received percutaneous coronary intervention (PCI) experienced MACCE reduction if 1-year LDL cholesterol (LDL-C) levels were below 70 mg/dL.
The findings, published in the Journal of the American College of Cardiology, “reinforce the need for LDL-C control to take full advantage of the benefits of a revascularization procedure, particularly for PCI,” wrote researcher Michael Farkouh, MD, of the University of Toronto, and colleagues.
“Patients with 1-year LDL-C levels >70 mg/dL experienced lower rates of MACCE when undergoing CABG compared with PCI, whereas patients with 1-year LDL-C <70 mg/dL had similar rates of MACCE with CABG or PCI,” they wrote.
The analysis included data from 3 large, U.S. government-funded coronary revascularization trials involving patients with type 2 diabetes and heart disease (BARI 2D, COURAGE and FREEDOM).
Current guidelines recommend aggressive reduction of LDL cholesterol in patients with type 2 diabetes and established coronary heart disease (CHD), but Farkouh and colleagues noted that achieving guideline-recommended targets for cholesterol, as well as glycemic and blood pressure control, has proven challenging in patients with type 2 diabetes.
They further noted that the goal of their pooled analysis was to explore the role of LDL cholesterol levels on cardiovascular events after revascularization in these patients, “to assess whether there was a graded effect of achieved LDL cholesterol on outcomes after 1 year, and whether there was a possible differential effect of LDL cholesterol reduction according to assigned intervention strategy.”
Farkouh and colleagues categorized patients from the 3 trials included in the analysis according to levels of LDL cholesterol achieved after the first year of follow-up after revascularization (<70 mg/dL; between 70 and <100 mg/dL; and ≥100 mg/dL).
The study authors followed 4,050 patients for a median of 3.9 years after the index 1-year assessment.
Patients whose 1-year LDL-C remained ≥100 mg/dL experienced higher 4-year cumulative risk of MACCE (17.2% versus 13.3% versus 13.1% for LDL-C between 70 and <100 mg/dL and LDL-C <70 mg/dL, respectively; P=0.016).
When compared with optimal medical therapy alone, patients with PCI experienced a MACCE reduction only if 1-year LDL-C was <70 mg/dL (hazard ratio: 0.61; 95% CI, 0.40-0.91; P=0.016), whereas CABG was associated with improved outcomes across all 1-year LDL-C levels.
The researchers noted that the results were in accordance with the recently published 2018 American Heart Association/American College of Cardiology Guidelines on the Management of Blood Cholesterol.
“According to these guidelines, our analysis comprises a combination of high-risk and very-high risk patients who should be prescribed high-intensity statin and other LDL cholesterol lowering therapies with a target LDL cholesterol of at least 70 mg/dL,” they wrote. “This is particularly important in patients who underwent revascularization with PCI, because no MACCE benefit was observed in these patients with 1-year LDL cholesterol levels >70 mg/dL.”
In an editorial published with the study, Eliano Navarese, MD, of Nicolaus Copernicus University Bydgoszcz, Poland, and colleagues wrote that the 1-year finding in PCI patients “underscore the importance of follow-up LDL cholesterol measurements, both as a risk stratifier and as an indicator for therapy adjustments.”
“Current guidelines provide no formal recommendation on when to check LDL-C after PCI. In this pooled analysis, approximately 24% of these patients who underwent PCI exhibited elevated LDL-C ≥100 mg/dL levels during treatment that were associated with adverse long-term outcomes,” they wrote.
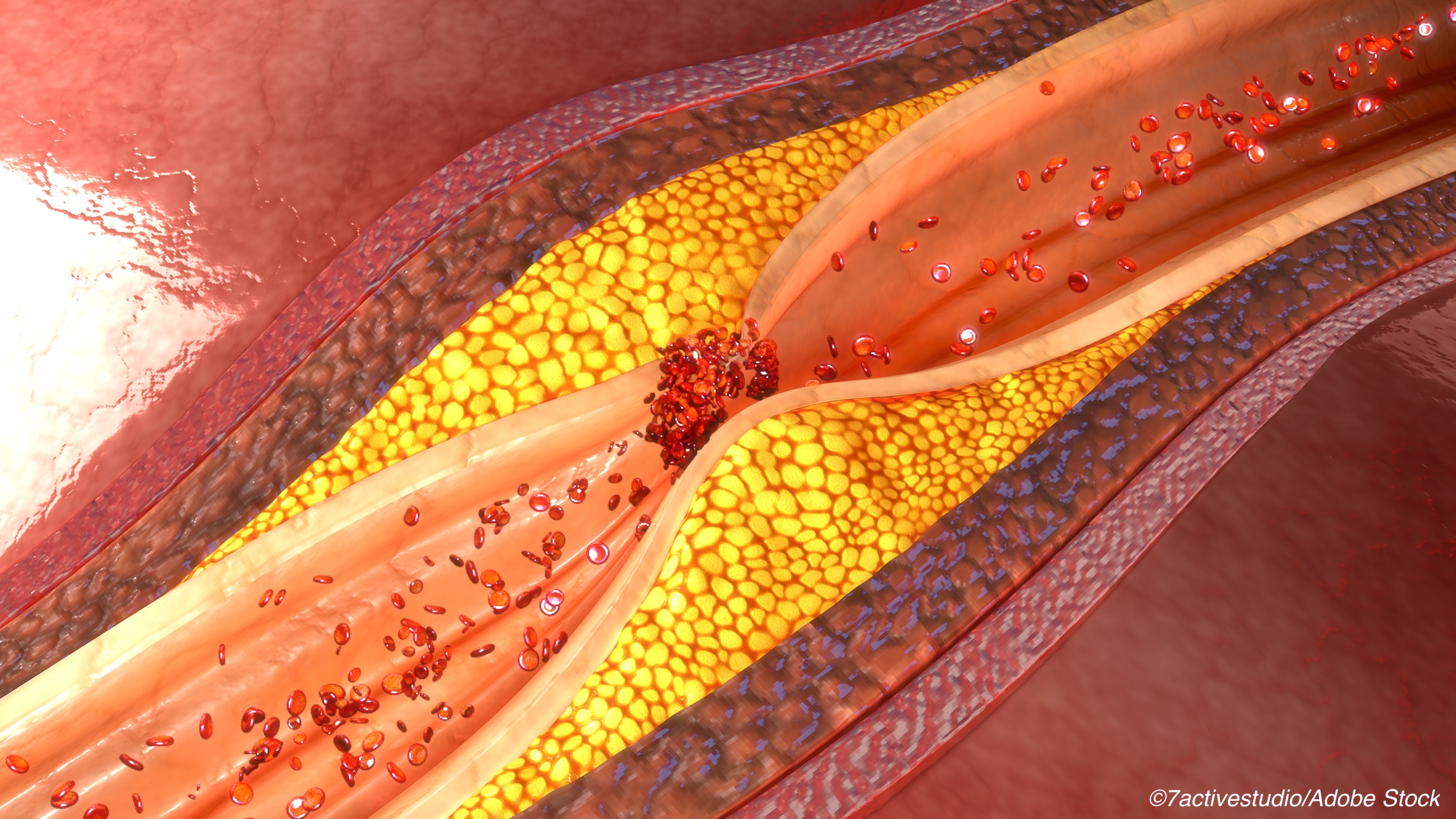
Navarese and colleagues noted that in addition to a patient’s clinical risk profile, LDL level “may be a marker of atherosclerotic burden and a surrogate of future plaque instability.”
“In this context, a baseline or on-treatment LDL-C threshold of 100 mg/dL might represent a vulnerable threshold of the atherosclerotic burden responsible for future events,” they wrote.
A study limitation identified by Farkouh and colleagues included the failure to randomize patients to different LDL cholesterol targets within the trials. In addition, the trials enrolled patients between 1999 and 2010, which may not reflect more contemporary clinical scenarios, and medical adherence to therapy was not recorded.
Despite these limitations, Navarese and colleagues concluded that the study findings “are relevant for clinical practice and may pave the way toward the generation of novel personalized medical models that can optimize care of patients with type 2 diabetes.”
“These models will ultimately integrate the treatment effects from coronary revascularization and lipid-lowering interventions with baseline and 1-year LDL-C thresholds,” they wrote. “This research is a much welcomed deeper foray into this important area and should increase the pace of future investigations to further unravel the so-far neglected association among LDL-C thresholds, outcome, and expected treatment effects in all high-risk subjects.”
-
In patients with type 2 diabetes and established heart disease undergoing revascularization, elevated LDL cholesterol level (≥100 mg/dL) was associated with an increased risk for major adverse cardiac or cerebrovascular events (MACCE) 1 year later.
-
Revascularization patients who received percutaneous coronary intervention (PCI) experienced MACCE reduction only when 1-year LDL cholesterol (LDL-C) levels were below 70 mg/dL.
Salynn Boyles, Contributing Writer, BreakingMED™
This research was funded by Gilead Science, the National Heart, Lung and Blood Institute, the Department of Veterans Affairs and the Canadian Institutes of Health Research.
Researcher Michael Farkouh reported receiving research grants from Amgen, Novo Nordisk, and Novartis. Researcher John Mancini reported receiving grants, honoraria, advisory board and speaking fees from Sanofi, Amgen, Boehringer Ingelheim and Novo Nordisk; and serving on the advisory board for Esperion.
Editorial writer Eliano Navarese reported receiving consulting fees/honoraria from Abbott, AstraZeneca, Amgen, Bayer, Sanofi, and Pfizer and Daiichi-Sankyo, unrelated to this editorial. Editorial writer Marc Brouwer reported receiving consulting fees/honoraria from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Pfizer, and Daiichi-Sankyo unrelated to this study.
Cat ID: 102
Topic ID: 74,102,102,4,12,192,669,94,916,918,925


