1. Compared to placebo, mitapivat was found to be effective in treating hemolytic anemia and increasing hemoglobin levels.
2. Mitapivat was found to be safe with acceptable adverse event profiles for patients.
Evidence Rating Level: 1 (Excellent)
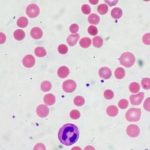
Study Rundown: Pyruvate kinase deficiency (PKD) is a rare hereditary disease highly associated with chronic hemolytic anemia due to mitochondria dysfunction, alongside serious complications such as pulmonary hypertension and thrombosis. Current management strategies are not curative and are associated with short- and long-term risks. Mitapivat is a first-in-class oral activator of red blood cell pyruvate kinase, approved by the FDA for treating hemolytic anemia in adults with PKD based on a previous phase 2 trial. The current study is a phase 3, multicenter, international, randomized placebo-controlled trial to assess the efficacy and safety of mitapivat in PKD patients who were not receiving regular red-cell transfusions. It was found that 40% of patients who received mitatpivat had an increased hemoglobin level, compared to none in the placebo group. Significantly more mitapivat recipients had a response in the improvement of hemolysis markers as well. While more patients who received mitapivat reported adverse events compared to placebo, none resulted in interruption or reduction of mitapivat dosage. Overall, this trial provided evidence for the efficacy and safety of mitapivat as the first disease-modifying oral treatment for PKD hemolytic anemia.
Click here to read the study in NEJM
Relevant Reading: Relevant Reading: Mitapivat Improves Ineffective Erythropoiesis and Reduces Iron Overload in Patients with Pyruvate Kinase Deficiency
In-Depth [randomized controlled trial]: The current study was a global, phase 3, double-blind, randomized, placebo-controlled trial to evaluate the efficacy and safety of mitapivat in 80 adult patients with PKD. Patients, 18 years of age or older were included if they had a confirmed diagnosis of PKD, a baseline hemoglobin level of 10.0g/dL, adequate organ function, and if they had not regularly received red-cell transfusions for the anemia. Patients were excluded if they were homozygous for the R479H mutation or had 2 non-missense mutations without another missense mutation in the PKLR gene, due to their lack of response to mitapivat in the phase 2 trial. Patients who had a splenectomy, or bone marrow or stem-cell transplantation, were also excluded. Patients were randomized 1:1 to receive mitapivat twice daily, starting at 5mg with the dose being escalated (up to 50mg) according to side effects and hemoglobin response, or a placebo. After 24 weeks, both groups were also eligible to participate in an open-label extension trial where all patients received mitapivat. Patients were stratified based on their PKLR mutations and baseline hemoglobin levels. The primary outcome was a hemoglobin response, defined as an increase from baseline of at least 1.5g/dL that was sustained throughout the study period. Secondary outcomes included average change from baseline and markers of hemolysis (indirect bilirubin, lactase dehydrogenase [LDH], haptoglobin) and hematopoiesis (reticulocyte proportion). Patients were assessed at 16, 20, and 24 weeks for these outcomes. Overall, 16 of 40 mitapivat recipients (40%) had a hemoglobin response, compared to none in the placebo group (adjusted difference, 39.3 percentage points; 95% confidence interval [CI], 24.1-54.6; P<0.001). Within patients who had a hemoglobin response, the mean (±SD) of the average change from baseline hemoglobin through 16, 20, and 24 weeks, was 3.5±1.4g/dL. Compared to placebo, the least-squares mean difference in hemoglobin change from baseline was 1.8g/dL (95% CI, 1.2-1.4), favoring the mitapivat group (P<0.001). In all stratified subgroups, patients treated with mitapivat had a greater response than those receiving placebo. Similarly, mitapivat recipients had greater responses in markers of hemolysis and hematopoietic activity than the placebo group. These improvements occurred early and were sustained through to week 24. Adverse events were reported in 88% of patients receiving mitapivat and 90% of those receiving placebo. The most common adverse events among mitapivat recipients were nausea (18%) and headache (18%), but their incidences were similar to or lower than those receiving placebo (23% and 33%, respectively). Adverse events of grade 3 or higher occurred in 25% of the mitapivat group and 13% of the placebo group. Serious adverse events occurred in similar numbers across both groups. However, none resulted in death, discontinuation, interruption, or dose reduction of mitapivat. Despite its small sample size, the inclusion of limited genetic variants, and short follow-up, the study provided evidence to support the efficacy and safety of mitapivat as a first-in-class disease-modifying therapy for adults with PKD.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.