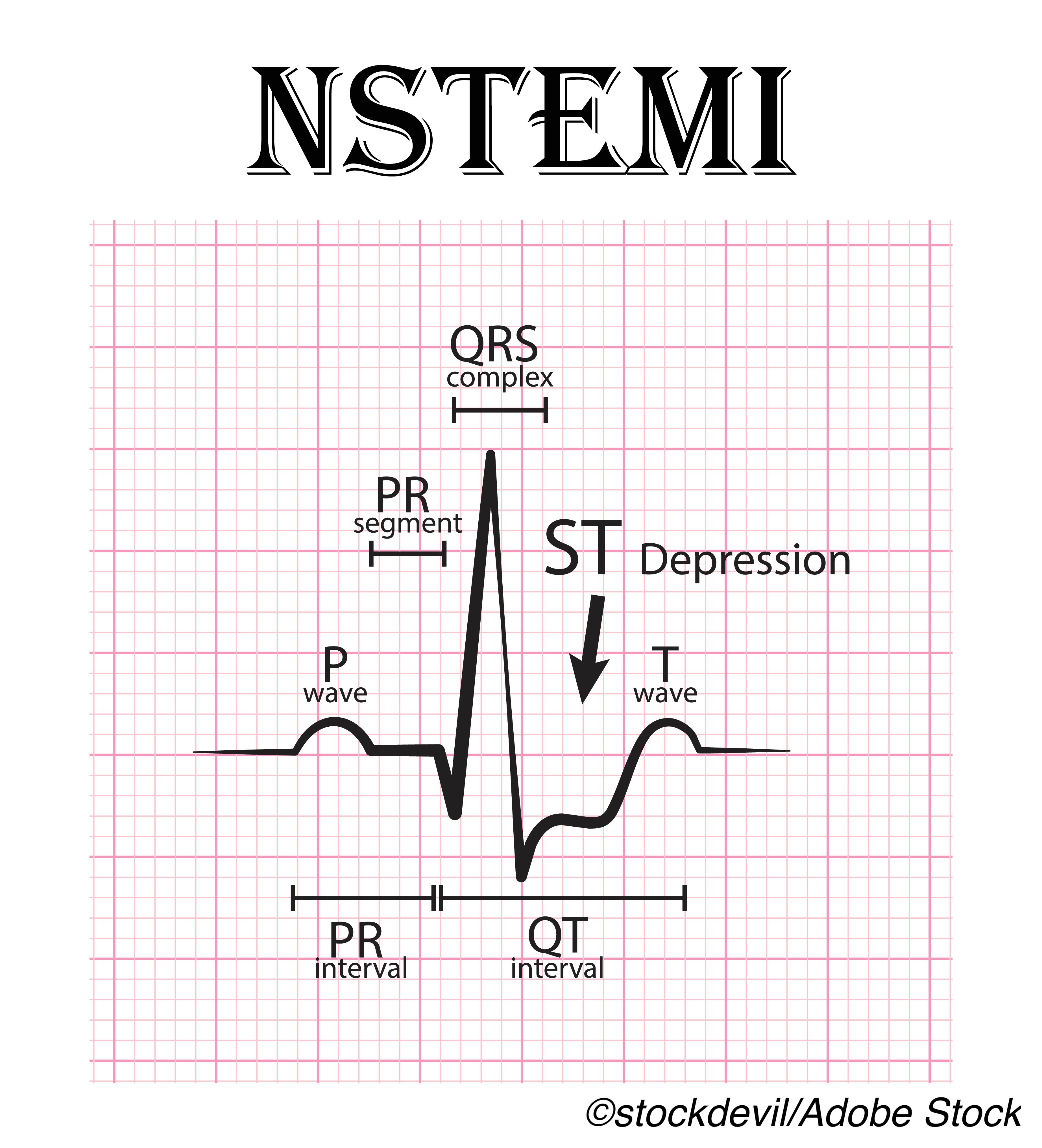
 Adjusted 5-year mortality in patients over 80 with non-ST elevation myocardial infarction (NSTEMI) was better with invasive management, the observational SENIOR-NSTEMI study found.
Adjusted 5-year mortality in patients over 80 with non-ST elevation myocardial infarction (NSTEMI) was better with invasive management, the observational SENIOR-NSTEMI study found.
Adjusted cumulative 5-year mortality was 36% in the invasive management group and 55% in the non-invasive management group (adjusted HR 0.68, 95% CI 0.55–0.84), according to Jamil Mayet, MD, of Imperial College in London, England, and co-authors. And, invasive management also was associated with a lower incidence of hospital admission for heart failure, compared with non-invasive management (adjusted HR 0.67, 95% CI 0.48–0.93), they reported in The Lancet.
“The survival advantage of invasive compared with non-invasive management appears to extend to patients with NSTEMI who are aged 80 years or older,” they wrote.
“Ideally, clinical decision making should be driven by findings from randomized trials,” they noted. “In the absence of randomized trial data, clinical decisions need to be made on the basis of the best available evidence. An invasive approach might be the better management strategy in patients who could be managed either invasively or non-invasively.”
In an accompanying editorial, Bjorn Bendz, MD, PhD, and Lars Aaberge, MD, PhD, both of Oslo University in Norway, wrote, “As [the authors] state, clinical decision making should be driven by randomized trials. However, will we ever have sufficient data from any study, independent of design or sample size, to guide clinical practice in very elderly patients?”
“Decision-making in older patients must be individually tailored, considering life expectancy, comorbidity, ischemic versus bleeding risk, cognitive and functional status (i.e., frailty), and patient preference,” they added. “We have a large number of possible treatment combinations in patients aged 80 years or older. Measuring quality of life and frailty by simple tests is possible but might be difficult to interpret. All newly acquired knowledge, including the results from the present study, could help to better assess the relation between benefit and risk for each individual when treating this challenging group of patients.”
Elderly patients with NSTEMI are less likely to be managed invasively. The 2008 GRACE study found angiography rates of 67% in people under age 70, compared with 33% in those over 80, and showed that revascularization was associated with 6-month mortality reduction when performed, with no increased stroke risk.
A 2019 analysis found increased use of coronary angiography in NSTEMI between 2004 and 2014, though the increase was proportionally higher in males 60 or younger, and reported that “lower adoption was noted in older, women and more comorbid patients. The risk-treatment paradox wherein patients who are most likely to benefit were less likely to receive coronary angiography persists even in contemporary practice.”
An ongoing randomized trial of invasive versus non-invasive NSTEMI management (SENIOR-RITA) in 2,300 patients 75 or older with 5-year follow-up and a primary outcome of the composite of cardiovascular death and non-fatal myocardial infarction is expected to be complete in 2029.
“According to present [2015] guidelines, medical optimization followed by an invasive strategy — including coronary angiography and subsequent revascularization with percutaneous coronary intervention or coronary artery bypass graft — is recommended for eligible patients with acute coronary syndromes without ST-segment elevation,” the editorialists observed. “However, these recommendations are not age-specific and have been based on registry studies, underpowered studies, or randomized trials of patients with mean age of around 65 years.”
In SENIOR-NSTEMI, Mayet and colleagues included 1,976 patients 80 or older from the U.K.’s National Institute for Health Research database who were diagnosed with NSTEMI between 2008 and 2017, excluding those who died within 3 days of peak troponin measurement and those with extreme propensity scores indicating very high likelihood of receiving one particular strategy over the other. Median age was 86 and 60% of the invasive and 50% of the non-invasive groups was male, respectively.
Ultimately, 686 patients in the invasive group and 892 in the non-invasive group were followed for intention-to-treat analysis at median 3-year follow-up.
Overall, 56% had non-invasive management. Predictors for non-invasive management included frailty and interstitial lung disease, while predictors for invasive management included inter-hospital transfer and family history of ischemic heart disease. Revascularization was done in 74% of the invasive group following coronary angiography.
Notably, there was no association between invasive management and lower mortality during the first month; the strongest associations were from one year of follow-up onward. “The association of invasive management with lower mortality appeared to attenuate with increasing age, but smaller patient numbers at the oldest ages meant that the confidence intervals on age specific HRs were wide,” the authors noted.
A recurrent acute coronary syndrome admission with invasive management during follow-up was seen in 5% of the invasive and 8% of the non-invasive group. Cumulative 5-year percentages admitted to the hospital with heart failure were 15% in the invasive group and 22% in the non-invasive group.
Limitations include those inherent to observational studies, with the inability to exclude bias due to residual confounding factors such as frailty, which may not be well-captured in routine clinical practice. In addition, outcomes for quality of life and independent living could not be assessed.
-
Adjusted 5-year mortality in patients over 80 with non-ST elevation myocardial infarction (NSTEMI) was better with invasive management (adjusted HR 0.68), an observational study found.
-
Invasive management was also associated with a lower incidence of hospital admission for heart failure, compared with non-invasive management (adjusted HR 0.67).
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was funded by the NIHR Imperial Biomedical Research Centre as part of the NIHR Health Informatics Collaborative.
The researchers declared no competing interests. The editorialists declared no competing interests.
Cat ID: 358
Topic ID: 74,358,282,494,730,358,192,925


