At the 2022 American College of Rheumatology Convergence meeting, Michael Pillinger, MD, presented his recent results from the PIVOTAL study. In particular, his analysis zoomed in on the neutrophil-to-lymphocyte ratio (NLR) and what that laboratory result may say about how gout flares result from an innate immune response against monosodium urate crystal deposits.1
The rationale for analyzing NLR stems from NLRP3 inflammasome activating the release of pro-inflammatory cytokines (eg, IL-1b), attracting and stimulating bloodstream neutrophils, including triggering neutrophil extracellular traps. Furthermore, an initial study has suggested that NLR may be increased in patients with active polyarticular gout.2 However, little is known about the relationship between NLR and gout flare in patients undergoing urate-lowering therapy or how treatment response influences NLR.
To address that question, Dr. Pillinger and colleagues assessed NLR in patients with gout at baseline prior to treatment with pegloticase (8 mg, 12 infusions) every 2 weeks in two parallel Phase 3 randomized trials, and thereafter at weeks 7, 13, 19, and 25. The urate-lowering response (serum urate <6 mg/dL for ≥80% of months 3 and 6) and flare status were measured.
The findings were derived from 36 pegloticase responders (72.2% men, aged 61.2±14.2) and 49 non-responders (85.7% men, aged 52.7±15.6). Baseline NLRs were similar between responders (3.39±2.73) and non-responders (4.23±2.80; P=0.132) and near or above the normal NLR range (0.78─3.533). In both groups, the NLR peaked in responders (4.59±5.62) and non-responders (4.94±5.40) at week 13, but by week 25, NLRs had all returned to baseline. Baseline NLR readings between patients who experienced flare (3.75±2.38) or no flare (3.55±2.14) were similar, although patients with flare had a significant NLR increase following therapy initiation, suggesting heightened systemic inflammation.
Dr. Pillinger and team concluded that sustained treatment to lower serum urate levels had little effect on NLR over the first 6 months of pegloticase therapy. Peak NLR occurred between weeks 13 and 19, although whether that is a consequence of flare or indicates a predisposition to flare is unknown. Rising NLR suggests that heightened systemic inflammation persists for weeks to months, and may contribute to renal, cardiovascular, or other disease states.
Physician’s Weekly spoke with Dr. Pillinger about his findings.
PW: Tell us about your study.
Dr. Pillinger: Pegloticase is a recombinant enzyme designed to lower serum urate. We humans, along with our closer primate relatives, lost this enzyme somewhere between 10 and 20 million years ago. Virtually all multicellular organisms have this enzyme, and they convert uric acid into allantoic acid, which is very soluble and easily excreted out of the kidneys. Better yet, allantoic acid tends not to form precipitates in the form of crystals when levels are high.
But we are the victim of a great cosmic joke, or maybe it was an evolutionary pressure that led us to lose this enzyme. As a consequence, our serum urates typically run somewhere between about 4.5 to 6.5 mg/dL, higher in men than in women, whereas your pet dog or cat has more like 1-2 mg/dL. That is actually a big and clinically meaningful difference. The fact that we lost this enzyme does not automatically give us gout, because that 4-6 mg/dL range is still below the solubility threshold, at least under most circumstances. However, when you add on to that baseline renal insufficiency, genetic factors of renal mishandling of soluble urate, or the impact of our modern diet of abundance that raises serum urate levels, that threshold gets pushed above the serum level of 6.8 mg/dL, which is the chemical precipitation solubility point. Once that happens, one can develop crystals, and hence, gout.
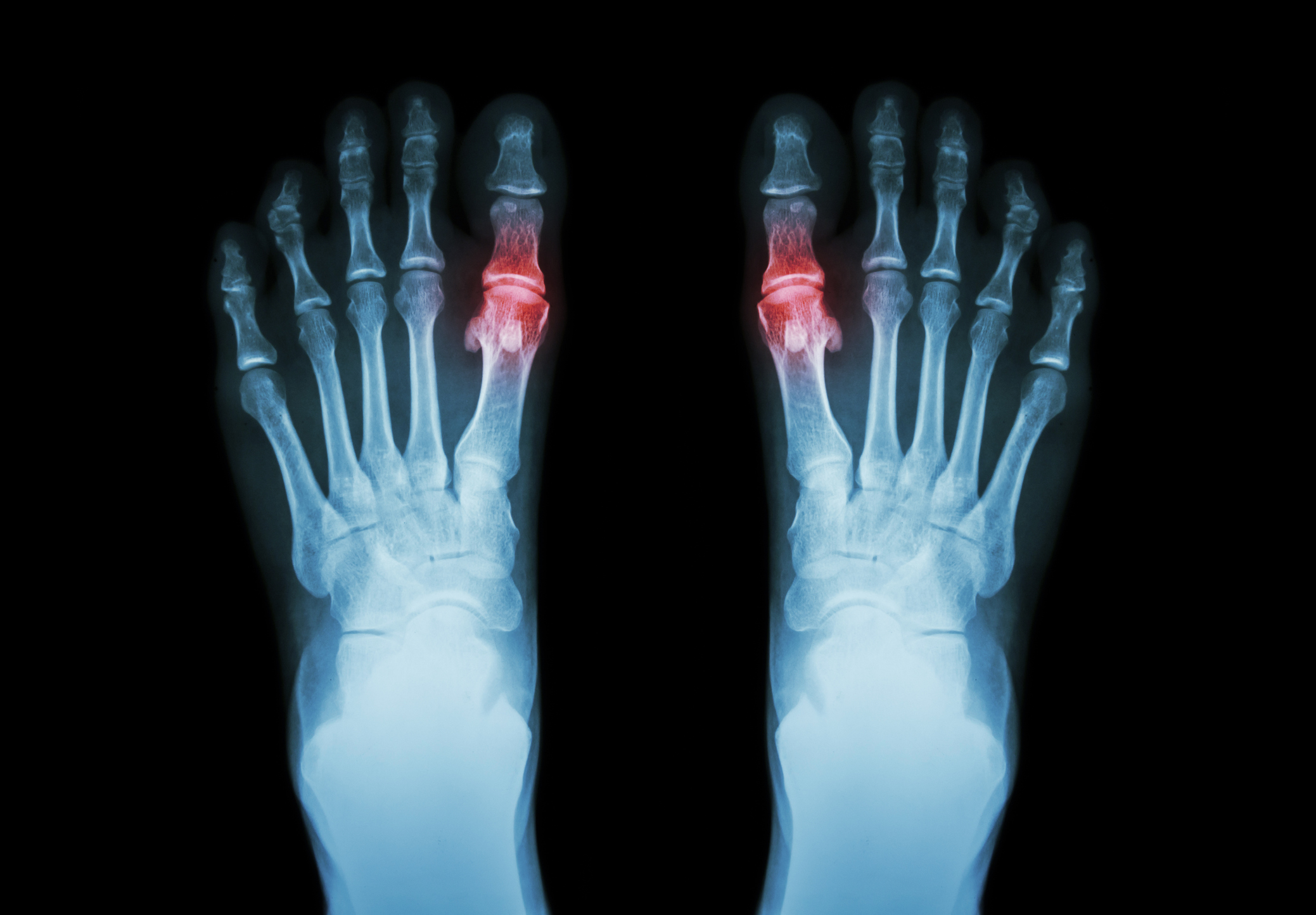
For rheumatologists, when that happens, there is a potent inflammatory signal; the crystals are perceived as a driver of an innate immune response. The characteristic appearance of gout, which is intermittent, is very acute flares that are painful, red, and hot. Nature or environment or whatever has led us to have an innately high urate that goes higher and then gets us into trouble.
PW: How is gout managed in general?
Dr. Pillinger: We use diet, which is partially helpful. The oldest drug that we have for lowering urate is allopurinol, which is an inhibitor of xanthine oxidase, and that is the enzyme that converts purines into uric acid, which is actually a purine itself. It stops the production of uric acid one step up the production line and is often very effective in many people. A newer drug called febuxostat, which acts at the same site, is uncompetitive instead of competitive, and is also effective in some people. A single drug that is approved to improve excretion of urate from the kidneys, is probenecid. In much of Europe, benzbromarone is approved and does the same thing but more potently; in the US, it was rejected by the FDA for hepatic toxicity reasons.
Some people don’t respond well enough to those drugs and still need care for quite bad gout with tophaceous deposits throughout their bodies. They often have some level of chronic kidney disease, which is common in gout in general, but even more common in the worst patients. We would like a therapy that could be more effective for those patients, and pegloticase has proven to be that therapy for some people. Pegloticase is a recombinant non-human mammalian uricase, which of course would be treated as a foreign antigen. Thus, it is surrounded by strands of polyethylene glycol to reduce immunogenicity, which does not completely solve the immunogenicity problem. The new solution to that problem is the use of immunomodulators to reduce the immunogenicity, typically the use of methotrexate as a co-therapy.
Let it be said that when pegloticase works, it works very, very well. We usually stop the drug as soon as we see it stop working, to reduce the infusion reactions. The two pivotal studies established the efficacy of the drug, demonstrating a remarkable benefit over placebo. That allowed us in this study to take a look at those two phase 2 trials and distinguish between patients who had a durable response and those who had a transient response and then lost response and were deemed a treatment failure.
PW: NLR: just a biomarker in gout or also part of the disease process?
Dr. Pillinger: I think you raise an interesting possibility; although we mostly think of NLR as a particular kind of biomarker, it may well participate in the process. NLR is used mostly by cardiologists and oncologists.3,4 Rheumatologists have not yet picked it up; we still live with our acute phase reactants as our primary readout of disease activity.
Part of the gestation of this project is actually to look at whether NLR can stand as a hallmark of inflammation. Given that this marker is about 10 or 15 years old, you might think somebody would have looked at it before, yet there is almost no data in our field.
Essentially, neutrophils function as acute phase reactants. Their numbers climb in the setting of various kinds of metabolic, endocrinologic, or infectious states, and they respond to all sorts of stress. Although lymphocytes might often be thought to serve as the equivalent of a housekeeping gene or a stable denominator, the data do not bear that out. In fact, under conditions of acute stress, of innate immunity for example, lymphocyte numbers actually fall. Consequently, the ratio between neutrophils and lymphocytes is a bit dynamic, and the interpretation goes beyond just comparing variable neutrophil numbers with stationary numbers of lymphocytes.
Although this is still exploratory, some collaborative work might suggest extrapolation from inflammation in gout and other chronic diseases. NLR elevation has been shown to predict various poor cardiovascular outcomes, including future myocardial infarction. After a percutaneous coronary intervention, for example, an intervention in the coronaries that had troponin rises, which is a bad marker of outcome. Given that troponin release during critical illness may be representative of systemic inflammation, it makes sense that rheumatology inflammation expertise would be relevant here.
PW: Why don’t we routinely measure NLR?
Dr. Pillinger: It is easy to derive, yet we don’t. One key part of our work reported at ACR Convergence was simply to look at the utility of NLR in a setting where we could observe closely. The first question was actually whether NLR would be altered by effective treatment.
I think our results are interesting and a little surprising, because there were no dramatic changes. Effective treatment did not seem to change NLR, in this study. However, our analysis suggests that there are probably some legitimate reasons.
We divided the study outcomes into responders and non-responders. Note that the so-called non-responders could have responded early but by 6 months had urate levels that drifted up again; it was not that one was inert. The serum urate at week 25 after treatment was 0.3, and the serum urate for non-responders was 8.9, demonstrating how effective pegloticase works. When we looked at the two groups and what happened to their NLRs over time with treatment, the NLRs rose at the first measurement points for both groups. Then the NLRs drifted down pretty much back to baseline over 25 weeks.
PW: Why did this happen?
Dr. Pillinger: In the placebo group, NLR did not change at all. Rheumatologists know that the urate lowering phase of gout treatment with any drug is actually pro-inflammatory and leads to flares. Some people call it crystal-stripping; people think that as urate dissolves from deposited areas, instead of simply melting away, it flakes off and goes to where it can drive inflammation. Probably what’s happening here is that inflammation is going up in the short term.
Instead of whether they responded or not, we looked at whether participants had no flares in the 6 months of observation, one to three flares in the 6 months of observation, or four or more flares in the 6 months of observation. Very roughly, the groups were similar. Remember that all groups had urate drops early on, before the non-responders’ urates rose. Everybody experienced urate fluctuations, whether they were responders or non-responders. The flares happened fast, mainly in the first and second month of treatment and then tailed off. We were able to look at the difference between a group that had no flares, a group that had limited flares, and a group that had many flares. This is where I think it gets pretty interesting, because in terms of NLR, there was a real difference. The group that had no flares had no increase in their NLR, it just kind of stayed flat. The group that had a few flares had an increase in their NLR, and the group that had the most flares had a bigger increase in their NLR. As a marker of gout flare inflammation, the NLR appears to work.
PW: Why is your data interesting?
Dr. Pillinger: Because it suggests something that was not at all evident when I was training. When I was training, there was an entity called inter-critical gout, which no longer exists in the gout nomenclature but clearly exists in your patients. It is just the word for gout between attacks and the definition of inter-critical gout was that everything goes back to normal.
Our data indicate that this seems not to be true here. After that early flare period, there is a persistent elevation of a relatively sensitive marker of inflammation, the NLR. There is almost no data on whether markers like CRP go up and persist. Again, just like the NLR, patients with gout tend to have higher CRPs than the general population, but there is almost no data about inflammation levels following one of these flares.
We seem to be seeing persistent inflammation after the peak of flares. These data do not yet let us look at the individual case; that is something I think we need to try to do. It suggests that the durable inflammatory response does not go away after that big toe or that knee isn’t swollen anymore.
From a cardiologist’s point of view, that’s really interesting and raises questions of risk. Data released this year say several interesting things about what happens when you’re in a persistent state of inflammation.
The flip side was a paper published in JAMA; a large population database showed that patients who have gout flares have a higher rate of myocardial infarction for approximately 60 days, and then their myocardial infarction risk goes back down to their baseline risk.5 I think our data is merging lanes with that observation because it is supporting the idea that there is a persistent inflammatory state that may represent a window of risk post-gout flare that we ought to be aware of. The gout flare never just affects the toe, and the fact that we are looking at the NLR—which cardiologists see as a marker for myocardial infarction—I think fits very nicely with that vision.
PW: Take-home messages?
Dr. Pillinger: We found that patients who received aggressive urate-lowering therapy had a transient NLR rise during the first 20 weeks, which then normalized as they were settled in at the end of the study. That was expected during flares, but what we now know is that NLR increases are also persist during the post-flare period. That may carry implications with regard to some of the bad outcomes that patients with gout experience. These data link inflammation from gout and inflammation as it activates the vasculature and probably the kidney. There’s a lot of discussion about that as well.


 Rebecca Shover
Rebecca Shover