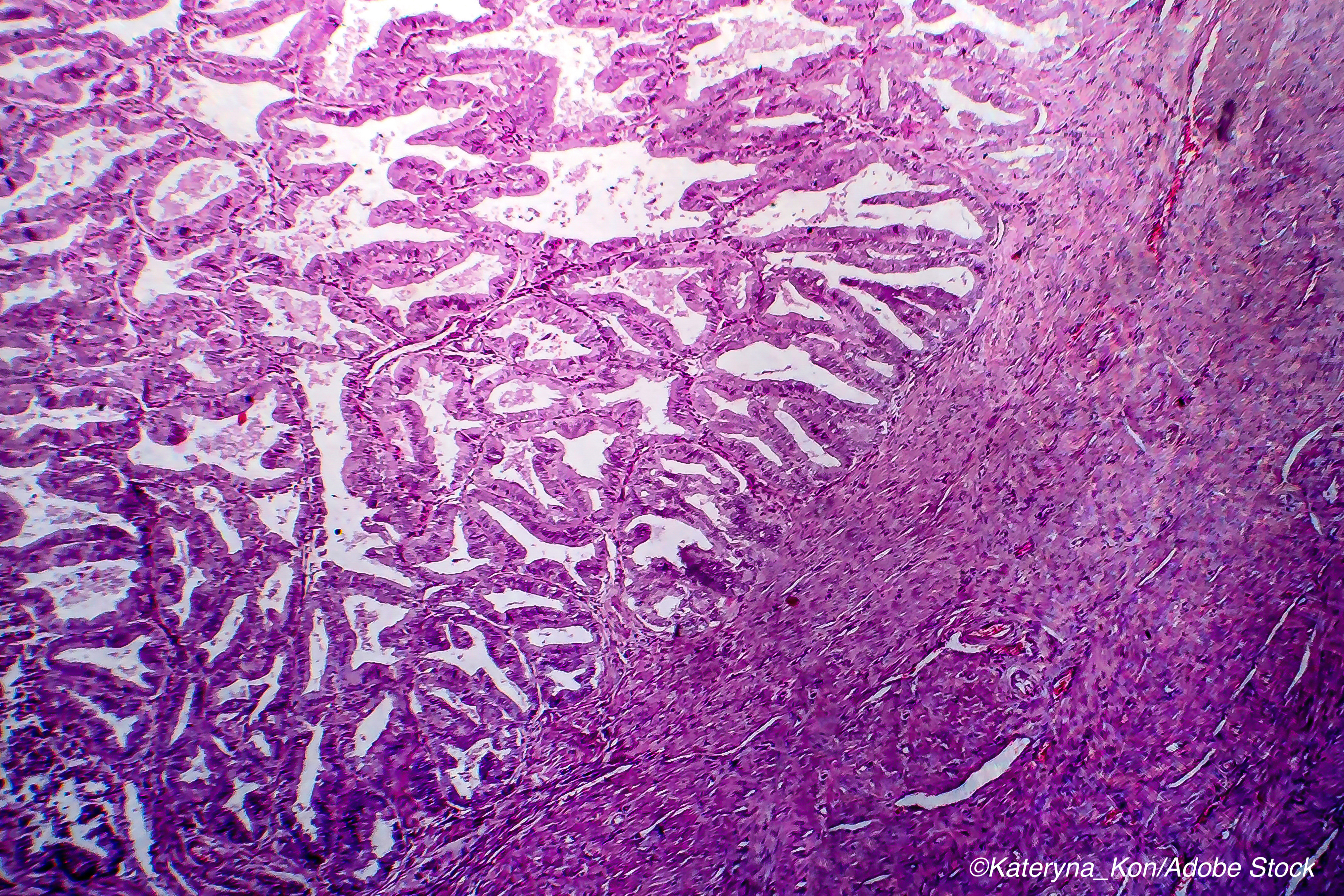
Among women with recurrent or advanced endometrial cancer (EC) who have undergone platinum-based chemotherapy and whose tumors are characterized by deficient mismatch mutation repair (dMMR), the anti-programmed death 1 (PD-1) monoclonal antibody dostarlimab appears to achieve a “clinically meaningful and durable antitumor” response with an acceptable safety profile.
That finding, which emerged from an open-label, non-randomized trial, suggests that the efficacy of PD-1 therapies depends upon the ability to target the deficient mismatch repair mechanisms that appear to sensitize endometrial cancers to those agents.
“The results of this analysis show that dostarlimab monotherapy was associated with an [objective response rate] ORR of 42.3% (95% CI, 30.6%-54.6%) for patients with recurrent or advanced dMMR EC that had progressed after treatment with platinum-based chemotherapy. Responses were durable, and with a median follow-up of 11.2 months, the median DOR was not reached,” wrote Ana Oaknin, MD, PhD, of Vall d’Hebron University Hospital in Barcelona, and colleagues in JAMA Oncology.
Currently, women with advanced or recurrent EC following standard chemotherapy face a grim prognosis, with treatment options limited to “salvage care with single-agent chemotherapy or hormone therapy, with limited clinical activity; response rates range from 7% to 14%, and median overall survival (OS) is less than 1 year.”
Because it is recognized that endometrial cancers have a high rate of dMMR, Oaknin and colleagues theorized that they would respond to treatment with a PD-1 antibody such as dostarlimab, an investigational agent that has high affinity to the PD-1 receptor.
The ongoing, open-label, single group, multicenter GARNET trial “began enrolling patients with deficient mismatch mutation repair endometrial cancer on May 8, 2017. Median follow-up was 11.2 months (range, 0.03 [ongoing] to 22.11 [ongoing] months; based on radiological assessments).”
Patients received 500 mg dostarlimab (IV) every three weeks for four doses, followed by 1,000 mg every six weeks until disease progression, treatment discontinuation, or withdrawal. The primary endpoint was objective response rate and duration of response as assessed by blinded central review.
As of July 2019, 104 women with dMMR EC were enrolled — of these, 71 had at least one measurable lesion at baseline and had completed at least six months of treatment at the time of data cut-off and were included in this efficacy analysis.
The median age was 64, and almost half (49.3%) had stage III or IV disease. All participants had at least one prior anticancer therapy; 64 patients had undergone surgery and 56 had received radiotherapy.
Among the findings:
- 30 of 71 patients had an observed response (ORR, 42.3% (95% CI 30.6-54.6%).
- 9 patients had a confirmed complete response (12.7%).
- 21 patients had a confirmed partial response (29.6%).
- Among the responders (n=30), 18 received one prior line of therapy and 12 receive two or more prior therapies.
- Disease control rate was 57.7%, and median progression-free survival was 8.1 months.
- Half of the responders (n=15) had achieved a response with prior platinum therapy.
“Responses were seen in 20 of 50 patients with type I EC (ORR, 40.0%; 95% CI, 26.4%-54.8%) and 10 of 21 patients with type II EC (ORR, 47.6%; 95% CI, 25.7%-70.2%). All patients with a confirmed complete response remained in response as of the data cutoff date,” they wrote. “In post hoc analyses, the ORR benefit of dostarlimab was observed across histologic subtypes, disease stages, and lines of therapy, although subgroup analyses were not powered and should be interpreted with caution.”
The safety analysis included all 104 enrolled patients, and the most frequently reported treatment-related adverse events (all ≥10%) were asthenia, diarrhea, fatigue, and nausea.
Oaknin and colleagues acknowledge several limitations, with the main one being the trial’s nonrandomized, single-group design, which makes statistical comparisons impossible. Also, the small sample size did not permit “robust subgroup analyses.” Also, patient selection was based on MMR status and did not include other biomarkers, “including PD-L1 expression level and tumor mutational burden.”
Nonetheless, the researchers concluded that the GARNET findings supported further study of dostarlimab. That additional research is ongoing and earlier this year, in a presentation at the 2021 American Society of Clinical Oncology Gastrointestinal Cancers symposium, researchers reported a 38.7% objective response rate for dostarlimab for treatment of non-endometrial solid tumors.
Moreover, dostarlimab recently received a positive review from the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA), but its FDA approval has been offset because inspections of manufacturing facilities where the drug is made have been delayed by Covid-19 issues.
In fact, the imprint of Covid-19 is omnipresent in all areas of oncology — from drug research to cancer diagnosis, according to Elizabeth J. Suh-Burgmann, MD, and colleagues of the Division of Gynecologic Oncology, The Permanente Medical Group, Division of Research, Kaiser Permanente Northern California, who looked at endometrial cancer diagnosis rates during the spring of 2020.
They compared weekly endometrial cancer incidence rates (diagnoses per 100,000 person weeks) from March to May and found that diagnoses declined by more than a third compared to the rate in 2019.
“From February 4 to March 3, the average weekly endometrial cancer incidence rate in 2020 (1.0, 95% CI 0.79–1.26) was similar to the rate in 2019 (0.94, 95% CI 0.74–1.19). Whereas the rate from March 4–May 26 remained stable in 2019 at 0.88 (95% CI 0.77–1.02), with 191 cancers detected, the rate in 2020 during the pandemic dropped to 0.58 (95% CI 0.48–0.69), with 127 cancers detected—a decline of 41% relative to prepandemic rates (incidence rate ratio 0.59, 95% CI 0.44–0.78, P <0.001) and 35% relative to the same period in 2019 (incidence rate ratio 0.65, 95% CI 0.52–0.82, P<0.001),” they wrote in a Research Letter published in Obstetrics & Gynecology. “Calls for abnormal bleeding preceded diagnoses in 41% of cases in 2020 compared with 35% of cases in 2019. However, the volume of calls about abnormal vaginal bleeding during the pandemic was 33% lower in 2020, at 52.8 (95% CI 51.9–53.8) compared with 78.5 (95% CI 77.3–79.7) in 2019 (incidence rate ratio 0.67, 95% CI 0.66–0.69, P<0.001).”
Covid-19 is still very much an ongoing public health concern, which may continue to feed into the fear that Suh-Burgmann and colleagues say is sparking delays in endometrial cancer diagnosis. Their findings “indicate a need to raise awareness among women not to delay evaluation of abnormal bleeding and to consider strategies such as routinely inquiring about abnormal bleeding in virtual visits.”
-
Be aware that this report discusses an investigational agent that is not yet FDA approved for clinical use.
-
In the efficacy analysis of a nonrandomized phase 1 clinical trial of dostarlimab, the confirmed objective response rate was 42%; 13% of patients had a confirmed complete response, and 30% of patients had a confirmed partial response.
Peggy Peck, Editor-in-Chief, BreakingMED™
The GARNET trial was funded by GlaxoSmithKline.
Oaknin reported receiving honoraria and consulting fees from AstraZeneca, Tesaro, GlaxoSmithKline, Clovis, PharmaMar, Roche, GenMab, Deciphera, Immunogen, and Mersana Therapeutics.
The study by Suh-Burgmann and colleagues was funded by the Permanente Medical Group Physician Researcher Program.
Suh-Burgmann and colleagues had no disclosures.
Cat ID: 120
Topic ID: 78,120,730,120,191,192,925,934


