The following is the summary of “Clinical and pathological features of anti-glomerular basement membrane disease associated with membranous nephropathy: an observational study” published in the November 2022 issue of Renal failure by Zhang, et al.
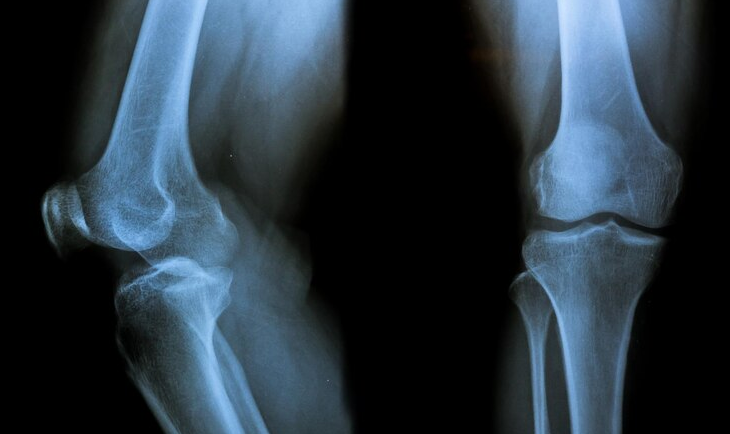
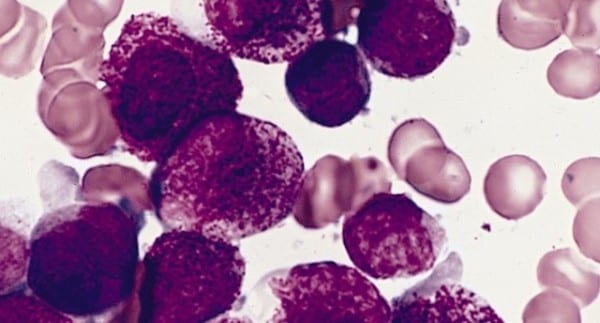
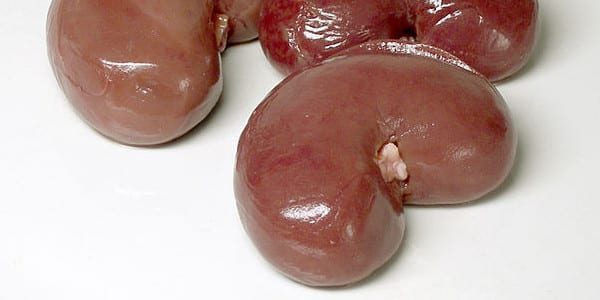
To learn more about anti-glomerular basement membrane (anti-GBM) illness and membranous nephropathy (MN), including its symptoms, causes, treatments, and outcomes in patients. About 7 patients were enrolled in this trial; all 7 had an anti-GBM illness and were also experiencing MN. Anti-GBM glomerulonephritis (GN) controls included 13 patients, and anti-GBM disease plus anti-neutrophil cytoplasmic antibodies (anti-GBM + ANCA) controls included 6 patients. Before immunosuppressive therapy or plasmapheresis was administered, laboratory tests and pathological data were evaluated.
The prognosis was evaluated during the course of the ongoing monitoring. Acute renal illness was seen in 28.57% of patients in the anti-GBM + MN group, significantly fewer than the 84.62% seen in the anti-GBM GN group (P=.022). There was no statistically significant difference between the percentage of patients who experienced hemoptysis among those who had anti-GBM and ANCA or MN (15.4% vs. 0%, P=.720) or those who did not have anti-GBM. Only 14% of those with anti-GBM + MN exhibited crescentic GN. In the anti-GBM + MN group, the necrosis rate was on average 29.0%.
Analysis of survival curves showed that patients who received (anti-GBM + MN) had better renal outcomes than those who received anti-GBM GN (P=.019). Anti-GBM GN was atypical in patients with both anti-GBM illness and MN. Early detection and treatment of anti-GBM illness linked with MN is necessary to improve renal recovery since these individuals had a smaller proportion of glomerular crescents and a better renal function prognosis than patients with conventional anti-GBM GN.
Source: tandfonline.com/doi/full/10.1080/0886022X.2022.2141645