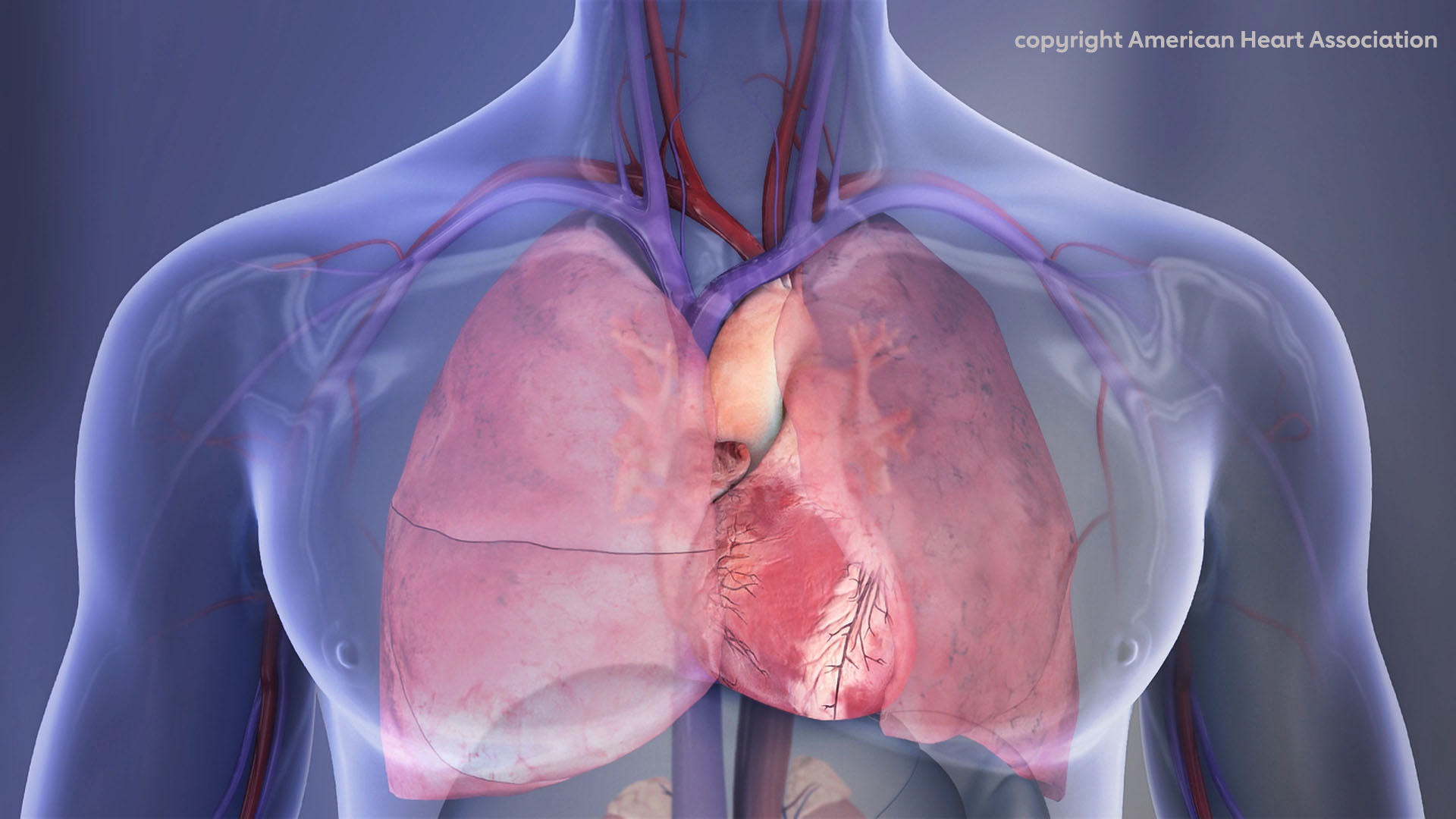
Patients with atrial fibrillation (AFib) and type 1 or type 2 diabetes may be less aware of symptoms of AFib such as irregular heartbeat, more likely to have lower quality of life, and have more comorbidities—including cardiac and neurological conditions—compared with patients with AFib without diabetes, according to a study published in the Journal of the American Heart Association.
Specifically, patients with diabetes were about 25% less likely to recognize the common symptoms of AFib compared with those without diabetes, three times more likely to be hypertensive, 55% more likely to have myocardial infarction, twice as likely to have heart failure, 75% more likely to have cognitive impairment, and had a 39% higher risk of stroke.
“Since diabetes is one of the major risk factors for AFib, our team investigated whether patients with and without diabetes differ in terms of atrial fibrillation symptoms and complications,” said Tobias Reichlin, MD, of Bern University Hospital, University of Bern, Switzerland, in a press release. “This research can provide insights on improving the management of atrial fibrillation and prevention of its complications.”
They included 2,411 patients (median age: 73.6 years; 27.4% female) with AFib from 14 health care centers in Switzerland enrolled in the Swiss Atrial Fibrillation (Swiss-AF) study. In all, 17.4% of these patients (n=420) had diabetes, but they were not classified according to type 1 or type 2 disease.
“Diabetes was defined on the basis of documented medical history and use of antidiabetic treatment. Participants were classified according to the use of antidiabetic medications into: patients without diabetes, patients with noninsulin-requiring diabetes, and patients with insulin-requiring diabetes. Participants were classified as having noninsulin-requiring diabetes if they had a diagnosis of diabetes and were on a diet and/or taking antidiabetic medications other than insulin/insulin analogues. Participants were classified as having insulin-requiring diabetes if they had a diagnosis of diabetes and were taking insulin/insulin analogues,” wrote Reichlin and colleagues.
Patients with diabetes were more likely to be older, smoke, and have a higher BMI, as well as a higher stroke risk compared with patients without diabetes (median CHA2DS2-BASc scores: 5 vs 3, respectively; P<0.001). The presence of diabetes was not associated with nonparoxysmal AFib (OR: 1.01; 95% CI: 0.81-1.27).
Compared with patients without diabetes, those with diabetes were less likely to perceive symptoms of AFib (OR: 0.74; 95% CI: 0.59-0.92) and more likely to have a worse quality of life (β= −4.54; 95% CI: −6.40 to −2.68). Patients with diabetes were also more likely to have the following comorbidities:
- Hypertension (OR: 3.04; 95% CI: 2.19-4.22).
- Myocardial infarction (OR: 1.55; 95% CI: 1.18-2.03).
- Heart failure (OR: 1.99; 95% CI: 1.57-2.51).
- Stroke (OR: 1.39; 95% CI: 1.03-1.87).
- Cognitive impairment (OR: 1.75; 95% CI: 1.39-2.21).
“It is remarkable to find that patients with diabetes had a reduced recognition of atrial fibrillation symptoms,” Reichlin said. “The reduced perception of atrial fibrillation symptoms may result in a delayed diagnosis of atrial fibrillation, and, consequently, more complications such as stroke. Our findings raise the question of whether patients with diabetes should be routinely screened for atrial fibrillation.”
“These important new findings from the large Swiss AFib study show compared to AFib patients without diabetes, those with diabetes were less likely to experience any symptom related to atrial fibrillation,” said Prakash Deedwania, MD, a member of the scientific advisory board for Know Diabetes By Heart (KDBH), a joint initiative of the American Heart Association and the American Diabetes Association, the immediate past chair of the American Heart Association Diabetes Committee and a professor of medicine at the University of California, San Francisco School of Medicine, in the same press release.
“These results were seen even though people with diabetes and AFib had more coexisting health conditions such as high blood pressure, as well as a history of heart attack and heart failure. Keeping these new observations in mind, along with the serious consequences of failing to recognize AFib in time, it seems prudent to consider screening older patients with diabetes for AFib so that treatment may be initiated when appropriate,” Deedwania concluded.
Study limitations include its cross-sectional design, the reliance on medical history rather than laboratory testing to determine a diagnosis of diabetes, a lack of data on diabetes duration and degree of glycemic control, and the lack of data on the generalizability of findings to other populations.
-
In this multicenter cohort study of patients with documented atrial fibrillation enrolled in the Swiss-AF study, researchers found that patients with diabetes less often perceive atrial fibrillation symptoms.
-
Patients with diabetes and atrial fibrillation were also more likely to have worse quality of life and more cardiac and neurological comorbidities than patients without diabetes.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
The Swiss-AF study is supported by grants from the Swiss National Science Foundation, the Swiss Heart Foundation, the Foundation for Cardiovascular Research Basel, and the University of Basel.
Reichlin has received research grants from the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, and the Cardiovascular Research Foundation Basel, all for work outside the submitted study. He has received speaker/ consulting honoraria or travel support from Abbott/ SJM, Astra Zeneca, Brahms, Bayer, Biosense-Webster, Biotronik, Boston-Scientific, Daiichi Sankyo, Medtronic, Pfizer-BMS, and Roche, all for work outside the submitted study. He has received support for his institution’s fellowship program from Abbott/SJM, Biosense-Webster, Biotronik, Boston-Scientific, and Medtronic, for work outside the submitted study.
Cat ID: 12
Topic ID: 76,12,730,2,446,913,12,192,669,918,925