1. Patients receiving pembrolizumab with or without platinum-based chemotherapy experienced longer progression-free and overall survival than the placebo group.
2. Pembrolizumab with or without platinum-based chemotherapy treatment was shown to increase overall survival compared to the placebo group.
Evidence Rating Level: 1 (Excellent)
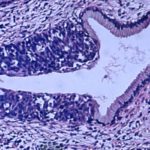
Study Rundown: Pembrolizumab is an immunotherapeutic that blocks anti-programmed death 1 (PD-1) to block tumor progression with demonstrated efficacy in cervical cancer. The study sought to investigate whether pembrolizumab would improve survival outcomes in cervical cancer patients receiving standard platinum-based chemotherapy. In this phase III randomized control trial, 617 patients with persistent, recurrent, or metastatic cervical cancer were randomized to either receive 200mg pembrolizumab or placebo treatment every 3 weeks for 35 weeks. Patients also concurrently received double platinum-based chemotherapy and at the investigator’s discretion, bevacizumab. The study found that patients receiving pembrolizumab experienced significantly longer progression-free and overall survival with increased effects observed in groups with greater PD-L1 combined positive scores. Administration of bevacizumab did not appear to influence the efficacy of pembrolizumab. The safety profile of pembrolizumab was as expected as previously reported with anemia and neutropenia being the most commonly reported adverse events. Together, this study supports the clinical use of pembrolizumab in the treatment of persistent, recurrent, or metastatic cervical cancer in parallel with a standard of care double platinum-based chemotherapy. While the study establishes the efficacy of pembrolizumab across the entire study cohort and in high PD-L1 expressing patients, it should be noted that when analyzed independently, the effect in the subgroup of patients expressing very low (<1) PD-L1 combined positive score cannot be confidently established.
Click to read the study in NEJM
Relevant Reading: Activity of Pembrolizumab in Recurrent Cervical Cancer: Case Series and Review of Published Data
In-Depth [randomized controlled trial]: In this double-blind, multi-center, parallel-group phase III randomized control clinical trial, 617 patients diagnosed with incurable cervical cancer who have not undergone systemic chemotherapy were enrolled into the trial. Patients were randomized in a 1:1 ratio into two groups: one receiving 200mg pembrolizumab intravenously every 3 weeks for 35 weeks and the other receiving placebo treatment. Patients also concurrently received standard of care paclitaxel and cisplatin/carboplatin chemotherapy, and at the investigator’s discretion, bevacizumab (15mg/kg). PD-L1 expression was assessed by biopsy sample. With respect to the primary endpoints of the trial, patients with PD-L1 combined positive score greater than one receiving pembrolizumab experienced significantly longer progression-free survival (10.4 vs. 8.2 months; hazard ratio [HR], 0.62; 95% confidence interval [CI], 0.5-0.77; P<0.001) and overall survival at 24 months (53% vs. 41.7%; HR, 0.64; 95% CI, 0.5-0.81; P<0.001). This effect was also observed in the entire cohort and the sub-cohort of patients with PD-L1 expression >10. Administration of bevacizumab was not a significant factor in survival. Patients receiving pembrolizumab also had a greater proportion of those responding to therapy, complete responses, and a longer duration of response. Grade 3-5 adverse events were observed more frequently in the pembrolizumab group (81.8% vs. 75.1%) with anemia, neutropenia, alopecia, and nausea being the most commonly reported. Patients receiving pembrolizumab also experienced a greater proportion of immune-mediated adverse events (33.9% vs. 15.2%). Taken together, this study supports the use of pembrolizumab for the treatment of cervical cancer.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.