The American Heart Association and the American College of Cardiology have updated their guideline on the prevention, detection, evaluation, and management of high blood pressure in adults for the first time in 14 years to redefine blood pressure (BP) levels. Under the new guideline, nearly half of American adults (46%) now classify as having high blood pressure.
Important Changes
High blood pressure (stage 1 hypertension) is now defined as systolic blood pressure (SBP) readings of 130-139 mm Hg, or diastolic BP (DBP) measurements of 80-89 mm Hg. That is a change from the previous definition of 140/90 mm Hg and higher, reflecting complications that can occur at those lower numbers.
The new guideline also eliminates the “prehypertension” category and redefines it as elevated/stage 1 hypertension. The previous stage 1 and stage 2 categories have now merged into stage 2 hypertension (Table). The new categories are defined as:
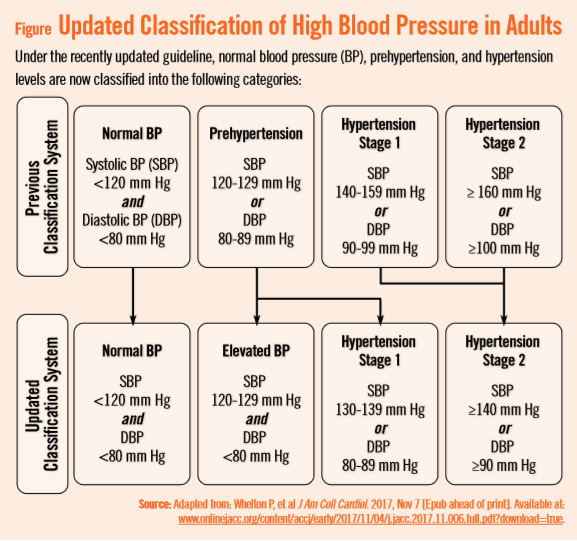
“Hypertensive crisis” is defined as SBP over 180 and/or DBP over 120, with patients needing prompt changes in medication if there are no other indications of problems, or immediate hospitalization if there are signs of organ damage.
About 4.2 million more people will be diagnosed with high blood pressure under the new guideline; however, only 1.9% more people will be advised to take medication, according to researchers.
Rather than immediate drug treatment, the guideline recommends that people with stage 1 hypertension first try lifestyle changes, such as exercising more, eating less salt, and eating more fruit, vegetables, and whole grains.
The guideline authors, though, stress that the new parameters are not simply about redefined numbers, but assessing the risk that goes along with having high BP.
“This is not a document to say, ‘What’s your number and are you above it or below it?’” says Don Casey, MD, MPH, MBA. “We wanted to take a look at all the existing and current evidence around hypertension related to BP and risks, classification of BP, measurement of BP, causes of hypertension, non-pharmaceutical interventions, patient evaluation, and more.”
Dr. Casey and colleagues used a risk calculator developed by the AHA to determine lifetime risk for patients developing high BP. “We’re now not just talking about a number, but about a patient’s risk. We’re trying to change the paradigm that above a certain number is bad and below a certain number is good.”
Other changes in the guideline include:
- Only prescribing medication for stage 1 hypertension if a patient has already had a cardiovascular event such as a heart attack or stroke, or is at high risk of heart attack or stroke based on age, the presence of diabetes mellitus, chronic kidney disease, or calculation of atherosclerotic risk.
- Recognizing that many people will need two or more types of medications for BP control.
- Identifying socioeconomic status and psychosocial stress as risk factors for high BP that should be considered in a patient’s plan of care.
A Team Effort
Dr. Casey says that management in accordance with guideline recommendations is effective only when followed by both practitioners and patients. Adherence to recommendations can be enhanced by shared decision making between clinicians and patients, with patient engagement in selecting interventions on the basis of individual values, preferences, and associated conditions and comorbidities.



 PhysWeekly
PhysWeekly