At Boston Medical Center, researchers learned in 2009 that their institution was a high outlier for postoperative venous thromboembolism (VTE). Their data were derived from the American College of Surgeons’ National Surgical Quality Improvement Program (ACS NSQIP) database. “After recognizing this fact,” says David McAneny, MD, “we implemented a standardized intervention for reducing postoperative VTE complications.”
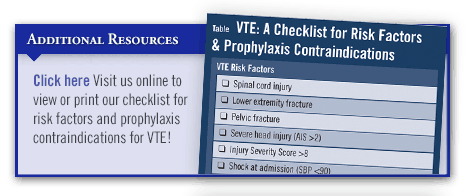
The intervention used standardized electronic physician orders to specify early postoperative mobilization and to mandate individualized VTE risk stratification for all patients. Patients must get out of bed and ideally walk at least three times daily, starting on the day of the operation when possible. Electronic order sets require VTE risk calculation before and after operations, and risk-stratified prophylaxis recommendations are automatically generated.
The system also provided reminders upon discharge for high-risk patients who warrant extended out-patient prophylactic anticoagulation. In-patient prophylaxis measures consisted of compression boots and/or heparin-based therapy, and out-patient low molecular weight heparin (LMWH) was administered to the two highest risk groups. The program also educated patients about the importance of VTE prevention.
Before & After
Dr. McAneny and colleagues conducted a trial, published in the Journal of the American College of Surgeons, in which VTE outcomes were compared for periods 2 years before and after implementing the program for patients undergoing general surgery or vascular operations. The frequency of DVTs was reduced by 84% at 2 years after the prevention efforts began when compared with baseline data. There were also 55% fewer cases of pulmonary emboli. Notably, risk-adjusted VTE outcomes steadily declined from an odds ratio of 3.41 to 0.94.
In addition, the study found that surgeon adherence to ordering recommended VTE prophylaxis was high. Compliance rates ranged from 100% for patients at low or moderate risk for VTE to 77% for those in the highest risk category. The other 23% had contraindications to extended courses of LMWH. When patients did not receive prevention in accordance with the recommendations, the electronic physician orders required an explanation of the deviation.
A Model Example
Dr. McAneny says that the success of the prevention effort by his research team was likely due to the combination of early mobilization and individualized risk assessment and prophylaxis. “We are greatly encouraged by the success of our VTE prevention program and believe that it can serve as a model for other medical centers,” he says. “Surgeons should consider using resources from the ACS NSQIP to reduce the likelihood of this relatively common and potentially life-threatening postoperative complication.”



 TimH
TimH