1. Rilzabrutinib was active and 400mg twice daily was identified as the dose for further testing with low-level toxic effects.
2. Rilzabrutinib showed a rapid and durable clinical activity for the management of immune thrombocytopenia.
Evidence Rating Level: 1 (Excellent)
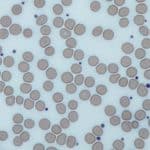
Study Rundown: Immune thrombocytopenia is an acquired autoimmune disorder characterized by immune-mediated platelet destruction and impairment of platelet production. The disease can increase a patient risk of bleeding, hospitalization, death, fatigue, and impaired quality of life. Rilzabrutinib, a BTK inhibitor, has been proposed to potentially increase platelet counts in patients with immune thrombocytopenia through decreased macrophage-mediated platelet destruction and reduced production of pathogenic autoantibodies. However, there is a gap in knowledge as to understanding Rilzabrutinib’s safe and effective dose in patients with immune thrombocytopenia to be further tested in phase 3 clinical trials. This study found that oral Rilzabrutinib led to rapid and durable clinical activity in 40% of patients with immune thrombocytopenia and that a 400mg twice-daily dose was identified to be safe and effective. This study was limited by no standard treatment recommendations that currently exist for patients with immune thrombocytopenia and by a range of time points and platelet-response endpoints. Nevertheless, these study’s findings are significant, as they identify a safe and effective dose for Rilzabrutinib to be used in an ongoing double-blind phase 3 trial comparing Rilzabrutinib with placebo in adults and adolescents with persistent or chronic immune thrombocytopenia, and demonstrate that oral Rilzabrutinib has a rapid and durable clinical activity.
Click to read the study in NEJM
Relevant Reading: Immune Thrombocytopenia Treatment
In-Depth [open label dose-finding clinical trial]: This international, adaptive, open-label, dose-finding, phase 1-2 clinical trial was conducted to evaluate Rilzabrutinib therapy in previously treated patients with immune thrombocytopenia, with 60 patients enrolled. Patients with immune thrombocytopenia who were aged 18 to 80 years, had a platelet count of less than 30×10^2 per cubic millimeter on two occasions and had a response to at least one previous therapy for immune thrombocytopenia were eligible for the study. Patients who were outside of the age range or did not have a response to previous therapies for immune thrombocytopenia, including splenectomy, were excluded from the study. The primary outcome measured was safety and platelet response, defined as at least two consecutive platelet counts of at least 50×10^3 per cubic millimeter and an increase from baseline of at least 20×10^3 per cubic millimeter. Outcomes in the primary analysis were analyzed via the Clopper-Pearson method and Kaplan-Meier analysis for time-to-event estimates. Based on the analysis, at the median of 167.5 days of treatment, 40% of the patients (24 patients) overall met the primary endpoint of platelet response. The median time to first platelet count of at least 50×10^3 per cubic millimeter was 11.5 days among all patients and 12.5 days among the patients who started Rilzabrutinib treatment at the highest dose of 400 mg twice daily. Among the group of patients with a primary platelet response, the mean percentage of weeks with a platelet count of at least 50×10^3 per cubic millimeter was 65%. Overall, this study demonstrated that a dose of 400mg twice-daily of Rilzabrutinib was shown to be safe and effective and that Rilzabrutinib provided a rapid and durable clinical activity in patients with immune thrombocytopenia, supporting the ongoing phase 3 trial that will better elucidate the magnitude and durability of clinical benefit with Rilzabrutinib treatment.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.