 Monotherapy with the Janus kinase inhibitor ruxolitinib brought about meaningful response in heavily pretreated patients with steroid-refractory chronic graft-vs-host disease (SR-cGVH) after allogeneic hematopoietic stem cell transplant, according to researchers from a small, single-site case series published in JAMA Network Open.
Monotherapy with the Janus kinase inhibitor ruxolitinib brought about meaningful response in heavily pretreated patients with steroid-refractory chronic graft-vs-host disease (SR-cGVH) after allogeneic hematopoietic stem cell transplant, according to researchers from a small, single-site case series published in JAMA Network Open.
Based on these findings, researchers concluded that ruxolitinib has the potential to become an option for these patients for whom there is no current standard-of-care treatment, but further study is needed.
“Allogeneic hematopoietic stem cell transplantation (HSCT) remains the sole curative treatment option for many patients with hematological malignant entities or bone marrow failure states. The population of patients undergoing allogeneic HSCT continues to increase because of expansion in the potential donor population achieved through the increasing use of both less than fully matched allogeneic donors and allogeneic HSCT in older recipients. The Center for International Bone Marrow Transplant Research estimated that the number of allogeneic HSCTs performed in the US increased to 9,028 in 2018; it is likely that more than 30,000 allogeneic HSCTs are performed worldwide annually,” wrote Joseph Clemente Alvarnas, MD, of the City of Hope Comprehensive Cancer Center, Duarte, California, in an accompanying editorial.
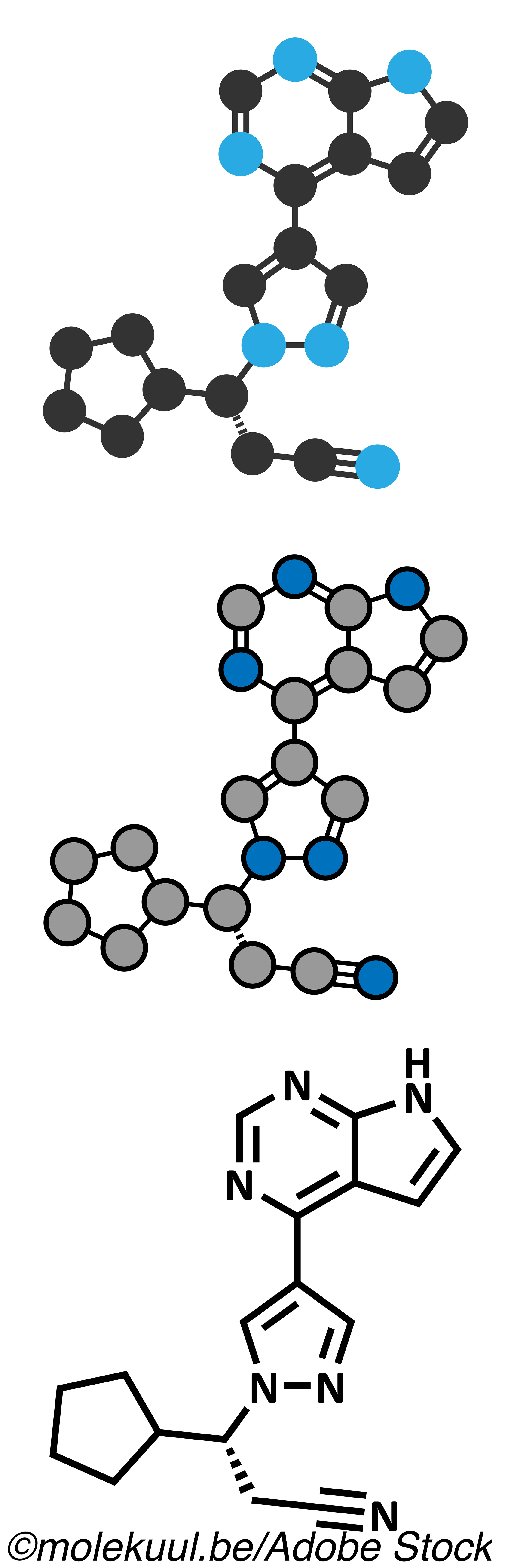
In patients who have undergone allogeneic HSCT, SR-cGVH is a significant cause of morbidity and mortality. In previous studies, ruxolitinib—a selective Janus kinase 1 and 2 inhibitor—has demonstrated promising results in the treatment of SR-cGVHD.
For this study, Hengwei Wu, MD, of Zhejiang University, Hangzhou, Zhejiang, People’s Republic of China, and colleagues included 41 patients (median age: 31 years; 34.1% female) treated with ruxolitinib for SR-cGVHD after undergoing allogeneic HSCT to determine treatment responses, factors associated with response, and adverse events during treatment administration. Patients were followed for a median of 14.9 months.
The two most common diagnoses included acute lymphoid leukemia (43.9%) and acute myeloid leukemia (41.5%). All peripheral blood stem cells were obtained from related donors. Patients received a median of three second-line immunosuppressive agents before treatment with ruxolitinib, with tacrolimus (87.8%) and mycophenolate mofetil (65.0%) being the most common. Treatment with ruxolitinib was begun at a median of 11.0 months after cGVHD diagnosis.
Oral ruxolitinib treatment was administered at 5 mg twice daily in patients weighing 60 kg or less, and 10 mg twice daily in those weighing >60 kg. Patients with grade 3 cytopenia were treated with 5 mg one daily. In those with worsening cGVHD within 4 weeks after administration, treatment was stopped. All patients were treated with prophylactic agents, including sulfamethoxazole for pneumocystis pneumonia and micafungin or posaconazole for invasive fungal disease.
In all, 36.6% of patients experienced complete remission, and 34.1% partial remission, for an overall response rate of 70.7% (95% CI: 56.2%-85.3%). Median time to response was 2 months. Ruxolitinib was continued for a median of 8.6 months in patients who responded. Overall response rates (ORRs) were similar in patients with moderate cGVHD and severe cGVHD (85.7% vs 63.0%, respectively; P=0.17), as was time to response (median: 2.3 vs 2.0 months; P=0.66).
All treated patients had a 6-month overall survival (OS) rate of 87.8% (95% CI: 77.3%-98.3%), and a 12-month OS of 65.9% (95% CI: 50.7%-81.0%).
Less favorable treatment responses were associated with lung involvement (OR: 0.112; 95% CI: 0.020-0.639; P=0.01) and matched related donors (OR: 0.149; 95% CI: 0.022-0.981; P=0.048).
Patients who received stem cells from a male donor (P=0.006), those who experienced complete remission before transplantation (P=0.02), those with moderate cGVHD at baseline (P=0.02), and those with skin cGVHD (P=0.001) demonstrated prolonged survival.
Major adverse events associated with treatment with ruxolitinib included cytopenia in 6 patients (1 with grade 4 thrombocytopenia) and infectious complications. Cytomegalovirus viremia was seen in 5 of 34 patients (14.7%), Epstein-Barr virus viremia in 19 of 36 patients (52.7%), 1 patient experienced reactivation of hepatitis B (2.4%), and 2 bacterial infection (4.9%). Femoral head necrosis occurred in 19.5%.
Recurrence of the underlying malignant neoplasm was seen in 14.6% of patients, and relapse occurred in 10.6% at 1 year, and in 17.1% at 2 years.
In conclusion, Wu and colleagues wrote: “This case series found that ruxolitinib in patients with SR-cGVHD had an ORR of 70.7% and CRR of 36.6%. Nearly all patients reduced the dose or discontinued the use of concomitant corticosteroids and other immunosuppressive drugs, minimizing their side effects and cost burden. Despite the limited sample size and retrospective nature, the results of this study indicated that patients with no lung involvement and haploidentical relatives as donors were more likely to benefit from ruxolitinib. Regarding the safety profile, the present study showed that infection events were the most severe adverse effect related to ruxolitinib, highlighting the significance of infection prophylaxis.”
Alvarnas, in his editorial, agreed, but offered some further caveats to the results.
“The advances put forth by Wu et al are welcome, but it is important to remember that patients with cGVHD require multidisciplinary care by a team that is experienced in the care of this unique patient population. Patients affected by cGVHD represent a unique population for whom a focus on distress management, infection monitoring, wound care, and management of the breadth of their care needs extends well beyond a single pharmacological intervention. By effectively integrating evidence-based advances in the care management of patients with cGVHD, including the use of agents such as ruxolitinib, into a multidisciplinary care delivery model, we can advance progressively toward a more effective, patient-centered set of care solutions for this unique population,” he concluded.
Limitations of this study include its observational, retrospective, single-center design and the limited number of patients included.
-
In this small, single-center study, monotherapy with the Janus kinase inhibitor ruxolitinib was associated with a meaningful response in patients with steroid-refractory chronic graft-vs-host disease, suggesting a possible therapeutic option for a serious disease with no currently accepted standard-of-care treatment.
-
Treatment with ruxolitinib was reasonably well tolerated with predictable and manageable toxic effects that included infectious complications and cytopenia.
E.C. Meszaros, Contributing Writer, BreakingMED™
This study was supported by the National Natural Science Foundation of China, the Key Research and Development Program of Zhejiang Province, and the National Science Foundation for Young Scientists of China.
Wu and Alvarnas reported no conflicts of interest.
Cat ID: 118
Topic ID: 78,118,728,791,730,118,119,468,192,925


