Short-course anticoagulant therapy proved non-inferior to a longer course in young patients (ages ≤21 years) with acute provoked venous thromboembolism (VTE), according to results from the Kids-DOTT trial.
In the randomized controlled trial conducted at 42 centers in five countries over 13 years among >400 patients, the Kaplan-Meier estimate for the 1-year cumulative incidence of the primary efficacy outcome was 0.66% (95% CI 0% to 1.95%) in the six-week anticoagulant therapy group and 0.70% (95% CI 0% to 2.07%) in the 3-month anticoagulant therapy group, reported Neil A. Goldenberg, MD, PhD, of Johns Hopkins All Children’s Hospital in St. Petersburg, Florida, and co-authors.
For the primary safety outcome, the incidence was 0.65% (95% CI 0% to 1.91%) and 0.70% (95% CI 0% to 2.06%), respectively, they stated in JAMA.
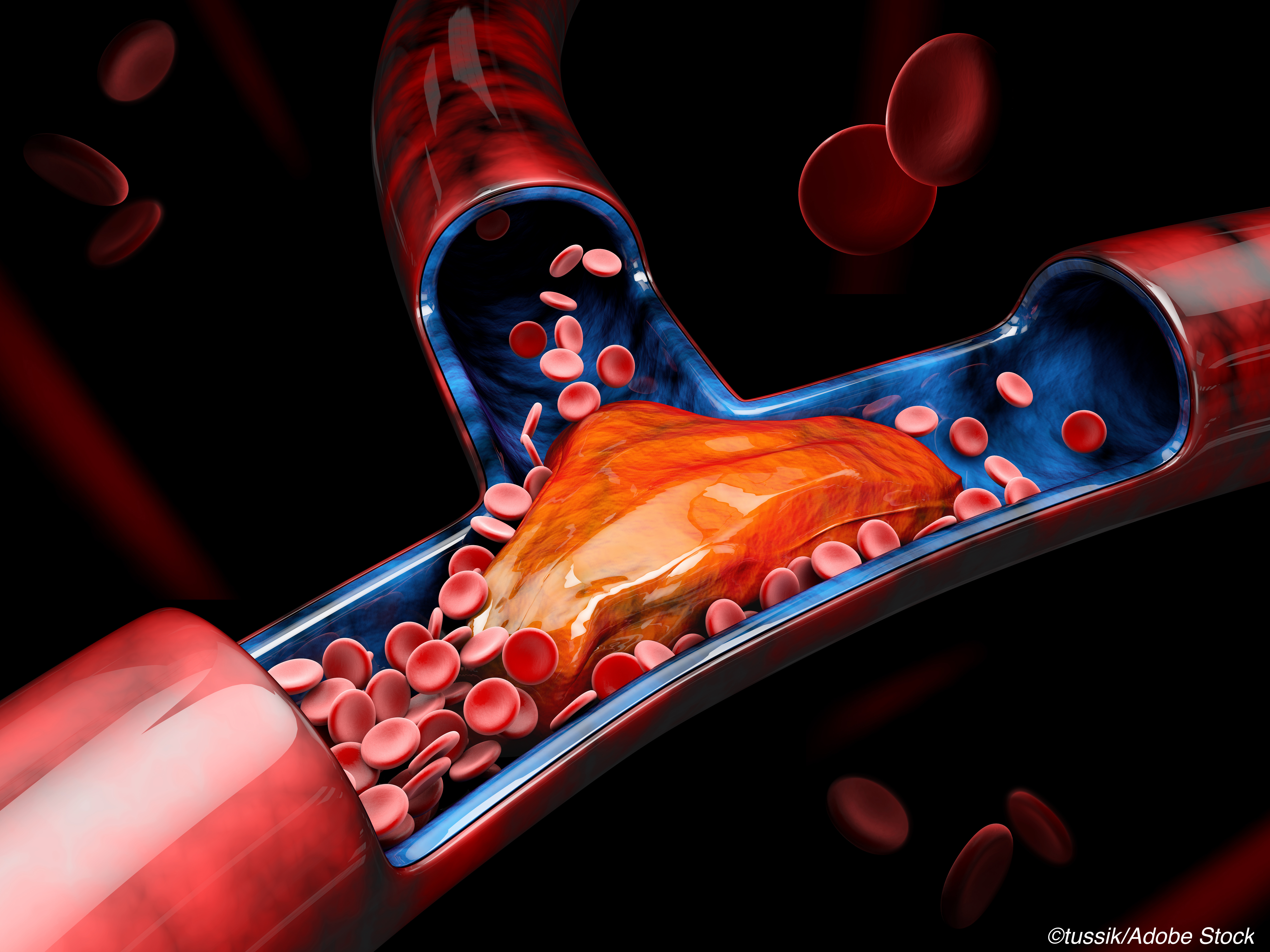
More than 90% of pediatric VTE cases are provoked, according to Goldenberg’s group. Risk factors for provoked VTE include those that disrupt at least one of the Virchow triad’s components, namely blood flow stasis, endothelial injury, and/or a hypercoagulable state, explained Jamie Shoag, MD, of Holtz Children’s Hospital in Miami, and co-authors. “Most children present multiple and simultaneous risk factors at the time of VTE diagnosis, including acquired (central line use, trauma, surgery, immobility, critical illness) and genetic thrombophilic conditions,” they wrote in a 2021 Pediatrics in Review article.
In a 2021 ThrombosisCanada lecture, Anthony K.C. Chan, MBBS, of McMaster University in Montreal, pointed out that other risk factors for pediatric VTE (ages 0 to 18 years) can be cancer and use of oral contraceptives.
While Kids-DOTT had some limitations—such as the predominant use of low-molecular-weight heparins (LMWH) even though direct oral anticoagulant therapies like FDA-approved dabigatran (Pradaxa), are used more often in “real-world” pediatric VTE—the authors emphasized that “anticoagulant therapy for 6 weeks compared with 3 months met noninferiority criteria based on the trade-off between recurrent venous thromboembolism risk and bleeding risk.”
Goldenberg and co-authors would certainly know, having studied the topic for some time. In a 2018 Expert Review in Hematology article, they offered a summary of the approaches to the duration of anticoagulation therapy in pediatric deep vein thrombosis (DVT), calling the future results from Kids-DOTT “critical to inform the future standard of care in pediatric VTE treatment.”
In a 2019 interview with Clinical Advances in Hematology & Oncology, Goldenberg explained that the incidence of VTE seemed to be on the rise, partly because of greater awareness among non-hematology physicians, and because the medical community is “providing invasive care to more children with critical illnesses and more children are surviving illnesses that were once fatal, which leads to more children with prolonged hospitalization in the intensive care unit with central venous catheterization and immobility, which increases the risk of VTE.”
Other research from the authors includes a 2019 analysis of the relationship between plasma coagulability and post-thrombotic syndrome in the Kids-DOTT biobank and a 2020 consensus recommendation for anticoagulant thromboprophylaxis in pediatric Covid-19-related illness.
In a 2021 Thrombosis and Hemostasis study, Goldenberg’s group sought, among other issues, to “define the incidence of rise in coagulability during the first 3 months post-provoked VTE,” and made the “novel observation of a marked rise in coagulability in 17% of children and young adults [n=90 patients ages ≤21 years] during the first 3 months postdiagnosis of provoked VTE, as measured by the maximal amplitude in the CloFAL [Clot Formation and Lysis] assay.” If validated, their “finding will have great potential to facilitate highly risk-stratified therapeutic approaches for provoked VTE in young patients,” the authors stated.
For Kids-DOTT (2008 to 2021), 297 children (median age 8.3 years; 49% female; around 80% White) met criteria for the primary per-protocol population analysis. In more than 38% of cases in both the short-course and long-course groups, placement of a central venous catheter was the “provoking factor” for index VTE. LMWH was used in 84% of the participants in the first week of treatment (acute) and in 86% during the subacute treatment period.
Patients could not have persistent antiphospholipid antibodies or complete occlusion on repeat imaging at 6 weeks. Follow-up was done to two years without routine surveillance imaging.
For primary analyses, the authors reported the following efficacy and safety, respectively:
- Kaplan-Meier estimates of the 1-year cumulative incidence of symptomatic recurrent VTE among all randomized patients (n=417): 1.03% (95% CI 0% to 2.43%) in the 6-week group; 1.60% (95% CI 0% to 3.38%) in the 3-month group for an absolute risk difference of −0.57% (95% CI −4.10% to 2.90%).
- Kaplan-Meier estimate of 1-year cumulative incidence of clinically relevant bleeding events among all randomized patients: 1.06% (95% CI 0% to 2.53%) and 2.47% (95% CI 0.31% to 4.59%), respectively; absolute risk difference of −1.41% (95% CI −5.19% to 2.28%).
For secondary analyses, Goldenberg and co-authors noted that “the 1-year incidence of postthrombotic syndrome itself among patients with index DVT of the limbs was similar in the 2 treatment groups for both the per-protocol population and all randomized patients… and excluded an absolute risk increase of greater than 14.7% for the postthrombotic syndrome in association with shortened anticoagulant therapy.”
Also, fever was the most common adverse event occurring in 26% of the six-week group and 32% of the three-month group.
Additional study limitations included the lack of patients with cancer and pulmonary embolism and the small number of primary efficacy and safety events.
Still, the authors pointed out that Kids-DOTT findings were in line with those from the EINSTEIN-Junior and DIVERSITY trials, although they cautioned that both had cases of unprovoked pediatric VTE, which is tied to an increased recurrence risk.
Guidance for managing this patient population is certainly out there. In 2011, Anthony K.C. Chan, MBBS, of McMaster University in Montreal, and Suzan Williams, MD, of the Hospital for Sick Children in Toronto, put out a management algorithm for neonatal portal vein thrombosis. Chan also worked on the American College of Chest Physicians (CHEST) 2012 guideline for anti-thrombotic therapy in neonates and children.
In 2018, the American Academy of Pediatrics offered its take on the evaluation and management of DVT in kids; while the American Society of Hematology (ASH) did the same with a 2018 clinical guideline. In an ASH YouTube presentation, Sarah O’Brien, MD, of Nationwide Children’s Hospital in Columbus, Ohio and the ASH pediatric VTE panel, explained that “one of the key recommendations…is how to approach a patient with asymptomatic thrombosis, meaning a blood clot that’s found incidentally on an imaging study…traditionally, pediatricians tend to treat most of these events…our recommendation…gives the physician the choice to anticoagulate or not to anticoagulate, and gives some scenarios, which may push a clinicians towards or away from anticoagulation.”
In 2020, the Children’s Oncology Group (COG) put out its own supportive care guidelines. While COG endorsed the 2018 ASH guidelines, they also cautioned that the latter’s advice for treating pediatric unprovoked VTE was conditional with “[v]ery low certainty in evidence.”
So will the latest results from Kids-DOTT change that? In a JAMA editorial accompanying the study, Jacques Lacroix, MD, of the Université de Montréal, and co-authors asked two other important questions: “Can these results be applied to all pediatric patients?” and “Should clinicians wait for the results of additional RCTs before changing the current guidelines?”
They reiterated that that “[f]ew patients with cancer or pulmonary embolism were enrolled in [Kids-DOTT] and patients with active malignancy were excluded. Further studies are needed to confirm the findings in these populations.”
As for their second question, given the scope of Kids-DOTT, it’s not likely to be repeated, Lacroix’s group stated, so clinicians can apply the results, but should do so “judiciously and not [extrapolate them] to patients with unprovoked venous thromboembolism and older patients.”
In their management algorithm, Chan and Williams suggested four initial steps: Rule out contraindication of anticoagulation therapy, minimize anticoagulation therapy, conduct repeat imaging, and perform long-term follow-up. “We should follow up these patients for at least five years, partly because most of the portal hypertension… is going to develop in the first three years,” Chan noted in the lecture.
-
In young patients (ages ≤21 years) with acute provoked venous thromboembolism (VTE) enrolled in the Kids-DOTT trial, anticoagulant therapy for three weeks versus for three months met non-inferiority criteria based on the trade-off between recurrent VTE and bleeding risks.
-
Clinicians should apply the findings from Kids-DOTT “judiciously,” and should not apply them to patients with unprovoked venous thromboembolism and older patients.
Shalmali Pal, Contributing Writer, BreakingMED™
Kids-DOTT was funded by the National Heart, Lung, and Blood Institute, Bridge Award/American Society of Hematology, Thrombosis Studies Award/Hemophilia and Thrombosis Research Society of North America, Eisai, and the Johns Hopkins All Children’s Foundation.
Goldenberg reported relationships with Anthos, Bristol Myers Squibb, Bayer, Daiichi-Sankyo, Pfizer, and Novartis. Co-authors reported relationships with, and/or support from, Bayer, Janssen Pharmaceuticals, EverlyWell, Virta, Wraser, Amgen, ARCA Biopharma, AstraZeneca/MedImmune, Better Therapeutics, CellResearch, Heartflow, Janssen, Novo Nordisk, Osiris, Regio Bio, HDL Therapeutics, Johnson & Johnson/Ortho-McNeil-Janssen, Boehringer Ingelheim, Grifols, Pfizer, Biomarin, Catalyst, Sanofi, Genentech, Octapharma, Takeda, Portola, Amarin, AstraZeneca, Servier, Idorsia, Merck, Novartis, Pfizer, PhaseBio, Regeneron, and Daiichi-Sankyo.
Lacroix and co-authors reported no relationships relevant to the contents of this paper to disclose.
Cat ID: 309
Topic ID: 74,309,730,309,139,192,925


