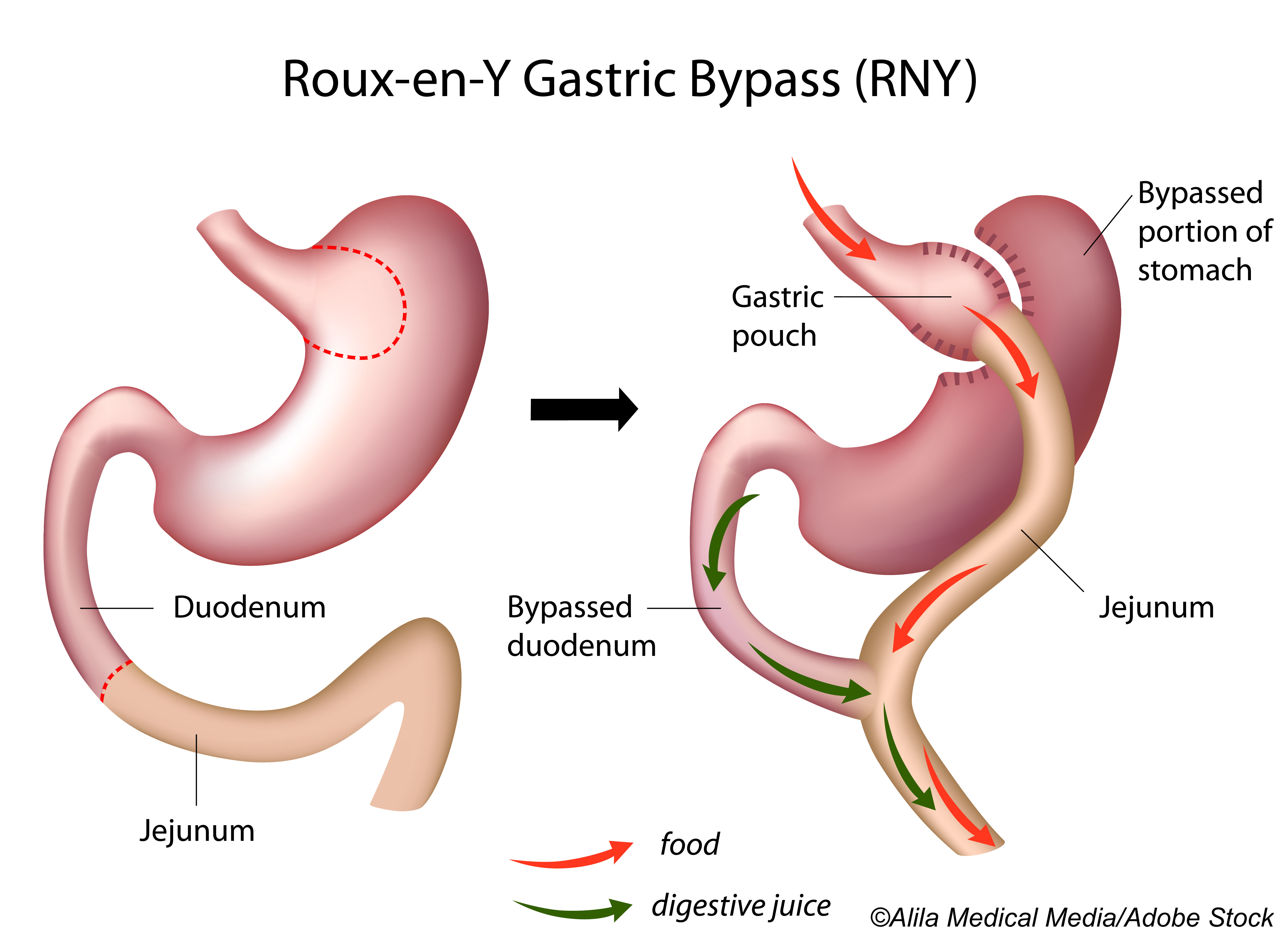
In patients with type 2 diabetes, both sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) procedures effectively reduced hepatic steatosis and brought about a nearly complete clearance of liver fat at one year, according to a recent study published in Annals of Internal Medicine. Both procedures, therefore, are appropriate in these patients to help minimize nonalcoholic fatty liver disease (NAFLD), researchers concluded.
“Nonalcoholic fatty liver disease (NAFLD), including hepatic steatosis, steatohepatitis, fibrosis, and cirrhosis, has a prevalence in the general population of about 25% and may progress to liver failure and hepatocellular carcinoma. Obesity, insulin resistance, hepatic steatosis, and inflammation are closely related, often coexist, and act synergistically with increased risk for cardiovascular disease. Moreover, a strong association between NAFLD and type 2 diabetes mellitus (T2DM) has been demonstrated, probably caused by hepatic insulin resistance. Hence, more than 90% of patients with obesity and T2DM may have NAFLD,” explained researchers led by Kathrine Aglen Seeberg, MD, of the University of Oslo, Oslo, Norway.
They conducted this single-center, randomized, controlled study to compare the effects of SG and RYGB on hepatic steatosis and fibrosis at one year among a cohort of 100 patients with type 2 diabetes (mean age: 47.5 years; 65% female; mean BMI: 42 kg/m2) from a tertiary care obesity center in Norway who had been randomized to undergo either SG (n=55) or RYGB (n=54).
Both groups of patients were required to adhere to a low-calorie diet of less than 1,200 kcal/d for two weeks postoperatively and were encouraged to maintain a healthy lifestyle throughout the study.
The primary outcome was remission of type 2 diabetes, and secondary outcomes included hepatic steatosis and fibrosis as assessed via MRI (liver fat fraction [LFF]), enhanced liver fibrosis (ELF) testing, noninvasive indices, and liver enzymes.
Mean baseline LFF was 19%, and at baseline, 24% of SG patients and 26% of RYGB had no or low-grade steatosis, defined as an LFF of 10% or lower. Reductions in LFFs were similar after both SG and RYGB procedures, with reductions of −19.7% (95% CI: −22.5% to −16.9%) and −21.5% (95% CI: −24.3% to −18.6%), respectively. At one year, 94% of patients who underwent SG and 100% of those who had RYGB had no or low-grade steatosis.
At baseline, 8% of SG patients and 6% of RYGB patients had severe fibrosis, defined as an ELF score of 9.8 or higher. At one year, these proportions were 9% and 15%, respectively (OR: 0.77; 95% CI: 0.16-3.62).
“Although there was great interindividual variation in the change in ELF score, overall, 18% of the patients demonstrated worsening and 5% an improvement of fibrosis, indicated by a higher or lower ELF category, respectively. However, most patients remained stable in the presurgical ELF category. The mean ELF scores were similar at baseline and 5 weeks in both groups but increased at 1 year by 0.21 (CI, 0.04 to 0.38) and 0.48 (CI, 0.30 to 0.65) after SG or RYGB, respectively; there were no substantial between-group differences,” wrote Seeberg and colleagues.
A full 77% of patients maintained persistent and stable ELF score categories, with only 18% experiencing worsening of fibrosis at one year. Researchers found no significant differences in this outcome between the two surgical groups.
Alanine aminotransferase (ALT) levels at one year had undergone significant reductions in SG patients (−17 U/L) and remained stable in RYGB patients (−4 U/L). There were no significant between-group differences at one year. Also at one year, aspartate aminotransferase (AST) levels had declined in both groups with no significant between-group difference. AST-ALT ratios were significantly higher in SG patients compared with RYGB patients, with a between-group difference of −0.18 (95% CI: −0.29 to −0.08).
Finally, researchers found significantly higher weight loss at one year in RYGB patients compared with SG patients (between-group difference: 8.4 kg; 95% CI: 0.3-16.4 kg). Also at one year, total and low-density lipoprotein cholesterol levels were significantly lower in RYGB patients compared with SG patients (between-group differences: −0.8 mmol/L and −0.7 mmol/L, respectively).
“In conclusion, RYGB and SG were both highly effective in reducing hepatic steatosis in patients with T2DM, with a substantial reduction in LFF 5 weeks after surgery and almost complete clearance of liver fat 1 year after surgery. Hence, both procedures stand out as appropriate treatment options to reduce the burden of NAFLD. The ELF test results might suggest a slight worsening in liver fibrosis after bariatric surgery, but further research is warranted on long-term progression or regression of fibrosis,” concluded Seeberg and fellow researchers.
Study limitations include its single-center design and inclusion of primarily White patients, short follow-up, non-generalizability of results to patients without type 2 diabetes, underpowering for secondary outcomes, the high number of secondary outcomes, and the exclusion of liver biopsy results to assess NAFLD.
-
Sleeve gastrectomy and Roux-en-Y gastric bypass procedures can both effectively reduce hepatic steatosis in patients with type 2 diabetes.
-
At one year postoperatively, patients with type 2 diabetes who underwent either procedure had almost complete clearance of liver fat.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was funded by the Vestfold Hospital Trust and the South-Eastern Norway Regional Health Authority.
Seeberg reported no disclosures.
Cat ID: 13
Topic ID: 76,13,730,13,795,111,192,518,917,925


